Tick-borne encephalitis – dangerous disease, which can have very serious consequences for a person, including death. Encephalitis is an insidious disease; a person can for a long time do not suspect that he is infected and do not take any action, because the incubation period of tick-borne encephalitis can reach 21 days.
Factors influencing the length of the incubation period
How long it takes from the bite of an infected tick to the appearance of signs of encephalitis depends on a number of factors. First of all, it depends on the state of the body of the bitten person. The better the protective system works, that is, the stronger immunity, the longer the so-called “infectious period”.
In children and older people, whose immunity is weaker, the incubation period for the development of diseases is shorter. With a very weakened immune system, signs of encephalitis may appear as early as 2 days after the bite.
There are cases when the body's immune defense is so strong that the symptoms of encephalitis never occur. The body successfully fights the virus, while producing antibodies, forming immunity to the virus. In this case, the only evidence that the body has been infected is a blood test that detects antibodies to encephalitis.
On average, the incubation period of tick-borne encephalitis lasts 8-14 days. The first symptom is fever - a rise in temperature to 38, sometimes up to 40 degrees. Weakness, chills, and weakness appear.
The duration of the incubation period of encephalitis also depends on the amount of virus that enters the body during the bite. Here a lot depends on how early the attached tick is detected. If little time has passed, then the tick most likely will not have time to transmit it to the human body a large number of virus. Quick detection and removal of an infected tick significantly reduces the likelihood of contracting encephalitis, but does not completely eliminate it.
The degree of infection depends on the correct removal of the tick. If the tick was crushed during removal, then there is a high probability that the entire virus contained in it will penetrate the wound at the site of the bite.
The sooner encephalitis is detected, the sooner treatment can begin and the more effective it will be. Therefore, if you are bitten by a tick, you should definitely consult a doctor and undergo necessary examination. Tick-borne encephalitis has an incubation period of 2 to 21 days, so early detection is the key to successful treatment.

When you see a doctor as soon as possible after a bite, the doctor will prescribe appropriate treatment, and the likelihood of complications is significantly reduced. The infected person is given immunoglobulin, which helps the body fight the virus. This fight is much more successful if the virus has not had time to multiply in the body.
Encephalitis is an inflammatory disease of the brain. There are primary encephalitis - epidemic encephalitis (Economo's disease), tick-borne (spring-summer) encephalitis, two-wave viral meningoencephalitis, leukoencephalitis (demyelinating encephalitis childhood) and secondary – influenza, malaria, measles.
Epidemic encephalitis (lethargic, Economo encephalitis, encephalitis A).
It was first observed in 1915–1916 in France and Austria in the form of epidemic outbreaks among soldiers. It was first described by Economo in 1917, and by Geimanovich and Raimist in 1920. After the first imperialist war in 1920–1926, there was a pandemic of the “classic form” of epidemic encephalitis.
The causative agent of this disease, a filterable virus, has not been isolated to date. The route of transmission of the virus is airborne droplets. IN acute stage in the brain matter it causes inflammatory process, affecting the hypothalamus, basal ganglia, nuclei of the oculomotor nerves. IN chronic stage a toxic-degenerative process develops, most pronounced in the substantia nigra and globus pallidus.
The clinical picture of epidemic encephalitis is characterized by a triad of symptoms:
General symptoms are headache, fever up to 38 degrees, malaise;
severe sleep disturbance - from drowsiness to soporous state from 7 – 8 days to a month or more;
oculomotor disorders: ptosis (drooping upper eyelid), diplopia (double vision), ophthalmoplegia (lack of movement eyeballs). Defeat is rarely possible facial nerve with the development of paresis of facial muscles, trigeminal nerve with pain in the face, isolated convulsions are possible.
Currently, the acute stage - lethargic or oculocephalic - has changed somewhat. Periods of drowsiness are followed by insomnia; drowsiness during the day and insomnia at night are observed. A vestibular form appeared - attacks with dizziness, nausea, vomiting, headache, photophobia.
Another modern variant is the pseudoneurasthenic form - irritability and weakness after a short illness with fever and mild oculomotor disturbances. The hyperkinetic form is a short acute period (headache, fever, drowsiness) and after 1-3 months convulsions appear, violent movements - twitching, hiccups, worm-like movements of the fingers, turns - twitching of the head. This form has a particularly severe course. Influenza form - erased acute period - 1-2 days influenza state and then parkinsonism gradually develops.
The chronic stage of epidemic encephalitis is the development of parkinsonism (from several weeks from the disease to 1 - 2 years). Changes in muscle tone gradually increase, which leads to a slowdown and impoverishment of movements (brady- and oligokinesia). Subsequently, trembling, trembling-rigid or akinetic-rigid forms of parkinsonism or their combination with various disorders sleep. The patient's movements are constrained, the head and hands are trembling, there is no facial expression, increased salivation, slow monotonous quiet speech, greasy face, mental disorders are possible.
Currently, the disease is rare and has an atypical course. They get sick at any age, but more often young people – 20-30 years old.
Treatment of epidemic encephalitis
Patients are subject to mandatory hospitalization. The incubation period has not been established precisely, so persons in contact with the patient are observed for 3 months. Specific treatment does not exist to this day. Symptomatically prescribed antivirals, hormone therapy, dehydration, B vitamins, antiallergic drugs, atropine-like drugs, antispasmodics.
Prevention of epidemic encephalitis
For the purpose of prevention, the sick person must be isolated until the end of the acute stage, the room where he was, his objects and clothes must be disinfected.
Tick-borne encephalitis
Tick-borne encephalitis (spring-summer, taiga)– acute neuroviral infection, which is transmitted by ticks, characterized by an acute onset, fever and severe damage nervous system.
This disease was described in 1934 - 1939 by A.G. Panov and M.B. Krol. The causative agent, a filterable virus, was discovered in 1937 by L. A. Zilber. E.N. Levkovich. The disease occurs in the Far East, Siberia, the Urals, Volga region, Belarus and a number of European countries.
Tick-borne encephalitis belongs to the group of natural focal human diseases. The main reservoir and carrier of the virus are ixodid ticks.

An additional reservoir can be rodents - hare, hedgehog, chipmunk, field mouse, birds - thrush, goldfinch, finch, predators - wolf. A person becomes ill through a tick bite; it is also possible to become infected through eating raw milk from goats and cows.
Symptoms of tick-borne encephalitis
The incubation period is 10 – 31 days. The virus enters the blood and nervous system and encephalitis develops. Heat– up to 40 degrees, severe headache, muscle pain, possible disturbance of consciousness, chills, nausea and vomiting, sleep disturbances. Acute period – 6 – 14 days. There is redness of the skin of the patient's face and chest, and the blood vessels of the eyes. Possible development of bronchitis, pneumonia, cardiovascular disorders vascular system and gastrointestinal intestinal tract. There are five clinical forms of the disease:
Feverish,
meningeal,
meningoencephalic
polio
polyradiculoneurotic.
The most favorable febrile form is 3-5 days of fever and mild neurological symptoms.
The most common form is meningeal - severe headache with meningeal signs (stiff neck, Kernig's sign - inability to straighten bent knees and hip joints legs). Lasts 7 – 14 days. The outcome is favorable.
The most severe form, meningoencephalic, has a high mortality rate of up to 20%. Symptoms of fever, meningeal symptoms are expressed, delirium, hallucinations are often observed, psychomotor agitation, epileptic seizures, hemiparesis, twitching.
In the polio form, patients develop paresis and paralysis of the arms and neck muscles against the background of fever - the arm falls, the head hangs on the chest, the affected muscles atrophy.
The polyradiculoneurotic form is characterized by damage peripheral nerves– pain along the nerves, tingling, numbness. It is less common than all other forms.
Examination after a tick bite
For diagnosis, a blood and cerebrospinal fluid test is taken. The main method - serological - diagnostic is an increase in antibody titer by 4 times.
Treatment of tick-borne encephalitis
Patients are hospitalized in infectious diseases hospitals.
For treatment, serum, immunoglobulin, antibiotics, dehydration, B vitamins, anticholinesterase drugs, and biostimulants are used. IN recovery period– additionally use neuroprotectors, massage, physical therapy.
The recovery period takes a long time. Residual effects are possible in the form of atrophy of the muscles of the shoulder girdle, Kozhevnikov epilepsy - twitching of a certain muscle group and periodic full-blown epileptic seizures.
Prevention of tick-borne encephalitis
Prevention of tick-borne encephalitis - protecting people from tick bites. This the right clothes(anti-encephalitis suits) in the forest, the use of tick repellents, self and mutual examinations after leaving the taiga. Ticks crawl up the grass in search of food - a bite site.

This is what a life-size tick looks like on the grass.
Therefore, you cannot walk barefoot or lie in the grass in the forest. A detected tick must be removed immediately. You can't crush him. It is better to immediately go to the emergency room of the nearest hospital or sanitary and epidemiological station. If this is not possible, remove the tick yourself by grabbing it (tweezers, a special device, thread) as close to the proboscis as possible and rotating it along its axis.

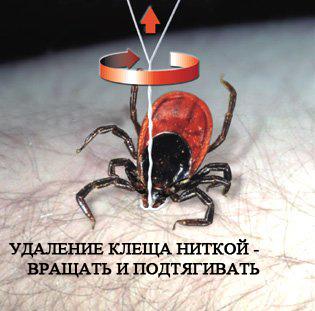
Don't pull too hard - you can tear it and get infected. The wound will need to be anointed with iodine.

The tick is examined in special laboratories for the presence of infection. It must be brought alive in a glass jar with a closed lid. Only 10 days after the bite can the blood be tested for tick-borne encephalitis. Persons exposed to a tick bite should be administered anti-tick immunoglobulin or prescribed antiviral drugs - anaferon, iodantipyrine, cycloferon, arbidol, remantadine. Active immunization of the population is carried out in the Primorsky Territory, the Urals, Altai, Latvia, Estonia ... - endemic foci. First of all, schoolchildren, pensioners - lovers of hiking, mushroom pickers and summer residents, people whose work involves traveling to the green zone - are vaccinated. 2 months should pass between vaccinations, and 3 weeks before going into the forest, so that immunity can develop. Educational work is being carried out with the population.
Double-wave viral meningoencephalitis
Two-wave viral meningoencephalitis is a peculiar clinical variant tick-borne encephalitis. Infection occurs through consumption of goat milk. The name is known - goat encephalitis. But infection is also possible through a tick bite. It is characterized by a short febrile period - 2 - 4 days, then the temperature decreases and after a few days rises again. The second wave is usually heavier than the first.
Seasonality July – September. The incubation period for infection with milk is 4–7 days, for a bite – 20 days. Encephalitis is milder, easier, and does not progress to the chronic stage. The current is favorable.
Influenza encephalitis – meningoencephalitis
Against the background of the flu, a sharp headache, dizziness, nausea, vomiting, meningeal signs, double vision, and drooping eyelids develop. In the severe form - hemorrhagic - the development of convulsions, hemiplegia, speech disorders, and motor coordination disorders is possible.
Treatment of influenza encephalitis
Treatment – antibiotics, dehydration, desensitization, vitamins. Medicines are prescribed by a doctor.
Prevention of influenza encephalitis
Prevention of the disease is the prevention of influenza - flu vaccinations, timely consultation with a doctor, increasing the body's defenses - immunostimulants, vitamins, good nutrition, the use of natural phytoncides - onions, garlic, lemons, limiting contacts and public events during the flu epidemic, the use of gauze bandages, the preventive use of oxolinic ointment.
Malarial encephalitis
Malarial encephalitis (Japanese, autumn, encephalitis B) - acute neuro viral infection, causing meningoencephalitis.
Its first epidemics with high mortality were recorded in 1871 in the Japanese cities of Kyoto and Osaka. Over the course of 100 years, Japan had several major epidemics of mosquito-borne encephalitis. It was only in 1934 that the causative agent, a filterable virus, and its carrier, the mosquito, were identified.
![]()
Natural foci of distribution are Japan, China, India, Korea, Vietnam, Africa, Java, the Philippines, the Far East and the Primorsky Territory.
The incidence of disease in humans depends on the activity of mosquitoes. The reservoir of the virus in nature is wild birds. They turn white at any age. After past illness strong immunity remains, meaning you cannot get sick twice.
When a mosquito bites the virus, it enters the bloodstream and spreads throughout internal organs. Thus, mosquito encephalitis is a generalized hemorrhagic capillary toxicosis.
The incubation period is 5 – 14 days, possibly up to 21 days.
Symptoms of malarial encephalitis
The onset of the disease is acute - high temperature (up to 40), headache, pain throughout the body, chills, nausea, vomiting, drowsiness, redness of the face, injections of eye vessels. After 3–4 days, the condition worsens further – meningeal syndrome increases. The pupils react sluggishly to light, there may be different sizes. There may be delirium, aggressiveness, which is replaced by drowsiness and coma. There may be convulsions, muscle tone increases, herpetic rashes may appear on the lips, breathing becomes impaired, and the pulse quickens.
A severe complication of this period may be cerebral edema with herniation into the foramen magnum, a drop in cardiac activity and death.
In the blood test, the content of leukocytes is increased, lymphocytes and eosinophils are decreased, and ESR is increased. with a favorable course of the disease, all symptoms regress, but the recovery process is long and difficult - 4-6 weeks. Possible neurological defects - paresis, coordination disorders, mental disorders leading to disability. Mortality rate – 40 – 70%.
To make a diagnosis, stay in an endemic area in the summer is taken into account. autumn period, clinical picture of the disease, serological tests of blood and cerebrospinal fluid.
Treatment of malarial encephalitis
For treatment, serum, specific immunoglobulin, resuscitation measures, detoxification, hormone therapy, neuroprotectors, anticholinesterase drugs, vitamins.
Naturally, such a disease can only be treated in a hospital with the presence of intensive care unit and all appointments are made by the doctor.
Prevention of malarial encephalitis
Prevention - anti-mosquito measures in areas where mosquito encephalitis is endemic, personal protective equipment against mosquitoes, vaccination, administration of immunoglobulin to those bitten.
Encephalitis due to infections
Encephalitis can develop with various infections, as their complication - herpes simplex, measles, chickenpox, rubella.
Rubella encephalitis occurs on the 3rd - 4th day of rubella rash.
The source of rubella is a sick child.
The causative agent is a virus.
Children get sick early age. May be congenital or acquired. Rubella is dangerous for pregnant women - risk of congenital malformations of the fetus - Greg's triad - damage to the cardiovascular system, eyes and hearing aid. The course is severe, mortality is high. High temperature, disorders of consciousness up to coma, generalized convulsions, epileptic seizures, hemiparesis.
There is no specific treatment. Symptomatically used corticosteroids, Lasix, nootropic drugs– encephabol, nootropil, cerebrolysin.
Measles encephalitis develops towards the end of the rash stage with a new wave of temperature rise and the development of coma, severe cerebral symptoms - headache, vomiting and focal symptoms of damage - paralysis, hyperkinesis (twitching), ataxia, loss of vision.
The causative agent of measles is a virus.
The route of transmission is airborne droplets.
Mostly children aged 2-5 years are affected. Mortality is high. After an illness, immunity is stable. During recovery, residual defects are possible - paresis, seizures, decreased intelligence. There is no specific treatment. Antibiotics are used anticonvulsants, nootropic, vitamins. Prevention – double vaccination of children aged 1 to 6 years.
All encephalitis is treated in infectious diseases hospitals. After suffering from encephalitis, in the chronic stage of encephalitis, you need to be observed by a neurologist, take a course drug treatment aimed at improving brain activity, restoration of motor, ataxic defect. In case of development of parkinsonism - permanent treatment– pramipexole (Mirapex), levakom, nacom, umex.
Consultation with a doctor on encephalitis
Question: if I am vaccinated against tick-borne encephalitis and am bitten by a tick, what should I do?
Answer: remove the tick; you do not need to take any medications.
Question: is the sanatorium indicated - spa treatment after suffering from encephalitis?
Answer: not shown during the first year. In the future, depending on the neurological deficit in the non-hot season.
Question: is it possible to distinguish an externally encephalitic tick from a non-infectious one?
Answer: no. Ticks infected and not infected with the encephalitis virus are absolutely identical in appearance.
Question: when traveling to which regions should you be vaccinated against encephalitis?
Answer: vaccination against Japanese encephalitis when traveling to the countries of South Asia and the Far East in late summer and early autumn, against tick-borne encephalitis when traveling to Austria, the Czech Republic, Karelia, the Urals, Krasnoyarsk and Khabarovsk Territories, Novosibirsk region, Volga region.
Each country has its own vaccination requirements for those arriving or departing from it. The World Health Organization annually publishes relevant requirements applicable to all countries.
If you are going on a trip abroad and do not know what vaccinations you need to get, you can contact the country's embassy, where they should give you all the necessary information.
Neurologist Kobzeva S.V.
- What is Tick-borne encephalitis
- Symptoms of Tick-borne encephalitis
- Treatment of tick-borne encephalitis
What is Tick-borne encephalitis
Tick-borne encephalitis(spring-summer encephalitis, taiga encephalitis) is a viral infection that affects the central and peripheral nervous system. Severe complications acute infection may result in paralysis and death.What causes tick-borne encephalitis
Caused by a filterable neurotropic tick-borne encephalitis virus. His clinical picture first described by A.G. Panov. The virus survives well low temperatures and is easily destroyed when heated above 70°C.
Russian virologists L.A. Zilber, M.P. Chumakov, A.K. Shubladze and others have isolated a large number of strains of the tick-borne encephalitis virus (in foreign literature it is rightly called Russian encephalitis), studied its properties, and established methods of transmission to humans. The transmitters of the virus and its reservoir in nature are ixodes ticks (Ixodes persulcatus). Refers to arbovirus infections (arboviruses - the term consists of the first syllables English words arthropodan borne viruses, which in Russian means “viruses transmitted by arthropods.” Blood-sucking arthropods include ticks, mosquitoes, midges, midges).
Pathogenesis (what happens?) during Tick-borne encephalitis
Human infection with the tick-borne encephalitis virus occurs during the blood-sucking of virus-forming ticks. The female tick's blood-sucking continues for many days, and when fully saturated, it increases in weight 80–120 times. Blood sucking by males usually lasts several hours and may go unnoticed. Transmission of the tick-borne encephalitis virus can occur in the first minutes of tick attachment to a person. Infection through the digestive and gastrointestinal tract when receiving raw milk from goats and cows infected with tick-borne encephalitis.
The seasonality of the disease is due to the biology of ticks, which appear in large quantities in the spring and summer. Diseases occur in many regions: in the Far East, Siberia, the Urals, Kazakhstan, Belarus, the Baltic States, the Carpathian, Leningrad and Moscow regions.
The virus enters the human body in two ways: through a tick bite and through nutrition. Nutritional contamination occurs when consuming raw milk, as well as dairy products made from the milk of infected cows and goats. When a tick bites, the virus immediately enters the bloodstream. However, with both methods of infection, the virus penetrates the nervous system hematogenously and through the perineural spaces. The virus is detected in brain tissue 2-3 days after the bite, and maximum concentration it is celebrated already by the 4th day. In the first days of illness, the virus can be isolated from the blood and cerebrospinal fluid. The incubation period for a tick bite lasts 8-20 days, for the nutritional method of infection - 4-7 days.
The duration of the incubation period and the severity of the disease depend on the quantity and virulence of the virus and on the immunoreactivity of the human body. Numerous tick bites are more dangerous than a single one. The course and form of the disease also depend on geographic features. Thus, tick-borne encephalitis in the Far East, Siberia, and the Urals is much more severe than in western regions Russia and countries of Eastern Europe.
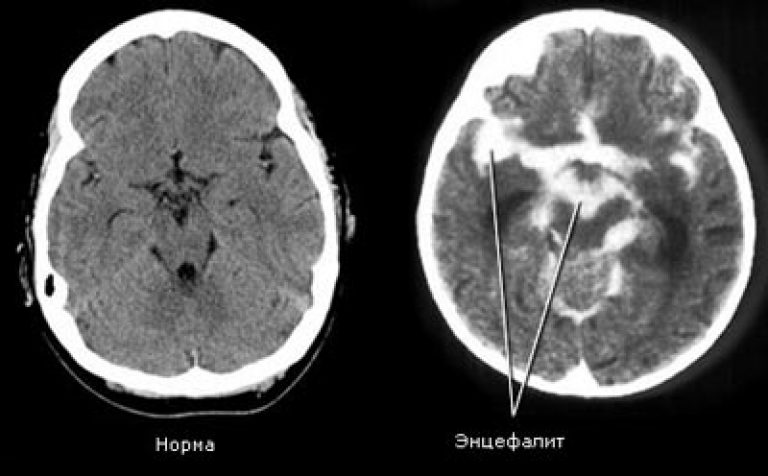
Pathomorphology
Microscopy of the brain and membranes reveals their hyperemia and edema, infiltrates of mono and polynuclear cells, mesodermal and glial reactions. Inflammatory and degenerative changes in neurons are localized mainly in the anterior horns of the cervical segments spinal cord, cores medulla oblongata, pons, cerebral cortex. Characteristic are destructive vasculitis with necrotic lesions and pinpoint hemorrhages. The chronic stage of tick-borne encephalitis is characterized by fibrous changes in the membranes of the brain with the formation of adhesions and arachnoid cysts, and pronounced glial proliferation. The most severe, irreversible lesions occur in the cells of the anterior horns of the cervical segments of the spinal cord.
Symptoms of Tick-borne encephalitis
Types of tick-borne encephalitis virus. IN Lately Russian specialists have adopted the division of tick-borne encephalitis viruses into three subtypes - Western, Siberian, Far Eastern.
The disease of tick-borne encephalitis in Europe occurs in more mild form than in the eastern part of the range of tick-borne encephalitis. For example, mortality in the European part of Russia in different years was 1–3%, and in the Far East, deaths occurred in 20–40% of those sick with tick-borne encephalitis.
Many researchers are inclined to believe that the severity of the disease depends on the ability of the virus to penetrate the blood-brain barrier, affecting or not affecting the brain.
Signs of tick-borne encephalitis. The incubation period of tick-borne encephalitis lasts on average 7-14 days with fluctuations from one day to 30 days. Transient weakness in the limbs, neck muscles, numbness of the skin of the face and neck are noted. The clinical manifestations of tick-borne encephalitis are diverse, and the course is variable. The disease often begins acutely, with chills and an increase in body temperature to 38–40°C. Fever lasts from 2 to 10 days. Appear general malaise, severe headache, nausea and vomiting, weakness, fatigue, sleep disturbances. In the acute period, hyperemia of the skin of the face, neck and chest, mucous membrane of the oropharynx, injection of the sclera and conjunctiva are noted. I am worried about pain throughout the body and limbs. Characteristic muscle pain, especially significant in muscle groups, in which paresis and paralysis usually occur in the future. Sometimes they are preceded by numbness, paresthesia and other discomfort. From the moment the disease begins, clouding of consciousness and stupor may occur, the intensification of which can reach the level of coma. Usually characteristic varying degrees stupor (stupor). However, the disease often occurs in mild, erased forms with a short febrile period. Often, erythema of varying sizes appears at the site of tick suction. However, the so-called migratory ring erythema is often a clinical marker of another infection - tick-borne borreliosis or Lyme disease, also carried by ticks.
Course of the disease. Despite the variety of manifestations acute period tick-borne encephalitis, in each individual case the leading syndrome of the disease can be identified. Based on this, and also taking into account the severity and persistence of neurological symptoms, five clinical forms of tick-borne encephalitis are distinguished:
1) febrile (erased);
2) meningeal;
3) meningoencephalitic;
4) poliomyelitis;
5) polyradiculoneuritis.
1) The febrile form of tick-borne encephalitis is characterized by a favorable course with fast recovery. The duration of fever is 3-5 days. Main clinical signs it is toxic-infectious manifestations: headache, weakness, nausea - with mild neurological symptoms. CSF values are without deviations from the norm.
2) The meningeal form is the most common form of tick-borne encephalitis. Patients complain of severe headache, worsening with the slightest movement of the head, dizziness, nausea, single or repeated vomiting, pain in the eyes, photophobia. They are lethargic and inhibited. Rigidity of the neck muscles, Kernig's and Brudzinski's symptoms are determined. Meningeal symptoms persist throughout the febrile period. Sometimes they are determined by normal temperature. The duration of fever is on average 7-14 days. In the cerebrospinal fluid there is moderate lymphocytic pleocytosis up to 100-200 per 1 mm3, an increase in protein.
3) The meningoencephalitic form of tick-borne encephalitis is observed less frequently than the meningeal form (the national average is 15%, in the Far East up to 20-40%). This form of tick-borne encephalitis has a more severe course. Delusions, hallucinations, psychomotor agitation with loss of orientation in place and time are often observed. Epileptic seizures may develop. There are diffuse and focal meningoencephalitis. With diffuse meningoencephalitis, general cerebral disorders are expressed (profound disorders of consciousness, epileptic seizures up to status epilepticus) and scattered foci organic damage brain in the form of pseudobulbar disorders (breathing disorders in the form of brady- or tachypne, according to the Cheyne-Stokes, Kussmaul type, etc.), uneven deep reflexes, asymmetric pathological reflexes, central paresis facial muscles and tongue muscles. With focal meningoencephalitis, capsular hemiparesis, paresis after Jacksonian convulsions, central monoparesis, myoclonus, epileptic seizures, and, less commonly, subcortical and cerebellar syndromes quickly develop. In rare cases (as a consequence of disturbances in the autonomic centers), a syndrome may develop stomach bleeding with bloody vomiting. Focal lesions are characteristic cranial nerves III, IV, V, VI pairs, somewhat more often VII, IX, X, XI and XII pairs. Later, Kozhevnikov epilepsy may develop, when general epileptic seizures with loss of consciousness appear against the background of constant hyperkinesis.
4) Poliomyelitis form of tick-borne encephalitis is observed in almost a third of patients. Characterized by a prodromal period (1-2 days), during which general weakness And increased fatigue. Then periodically occurring muscle twitching of a fibrillar or fascicular nature is detected, reflecting irritation of the cells of the anterior horns of the medulla oblongata and spinal cord. Suddenly, weakness may develop in any limb or a feeling of numbness may appear in it (in the future, severe motor disturbances often develop in these limbs). Subsequently, against the background of febrile fever (1-4 days of the first febrile wave or 1-3 days of the second febrile wave) and general cerebral symptoms, flaccid paresis of the cervicobrachial (cervicothoracic) localization develops, which can increase over several days , and sometimes up to 2 weeks. The symptoms described by A. Panov are observed ("head hanging on the chest", "proud posture", "bent, stooped posture", techniques of "torso throwing the arms and throwing back the head." Poliomyelitis disorders can be combined with conduction disorders, usually pyramidal: flaccid paresis of the arms and spastic - legs, combinations of amyotrophy and hyperflexion within one paretic limb. In the first days of the illness, patients with this form of tick-borne encephalitis are often sharply expressed pain syndrome. The most typical localization of pain is in the neck muscles, especially along the back surface, in the area of the shoulders and arms. Rise motor disorders with tick-borne encephalitis lasts up to 7-12 days. At the end of the 2-3rd week of the disease, atrophy of the affected muscles develops.
5) The polyradiculoneuritic form of tick-borne encephalitis is characterized by damage to peripheral nerves and roots. Patients develop pain along the nerve trunks, paresthesia (a feeling of “crawling goosebumps”, tingling). The symptoms of Lasseg and Wasserman are determined. Sensitivity disorders appear in the distal parts of the extremities of the polyneural type. Like other neuroinfections, tick-borne encephalitis can occur as Landry's ascending spinal palsy. Flaccid paralysis in these cases, they begin from the legs and spread to the muscles of the torso and arms. The ascent can also begin from the muscles of the shoulder girdle, involving the cervical muscles and the caudal group of nuclei of the medulla oblongata.
A fundamentally special variant is tick-borne encephalitis with a two-wave course. The disease is characterized by an acute onset, chills, headache, nausea, vomiting, dizziness, pain in the limbs, sleep disturbance, anorexia and the presence of two-wave fever. The first febrile wave lasts 3-7 days and is characterized by light current. There are moderate meningeal symptoms without damage to the cranial nerves. In the peripheral blood - leukopenia and accelerated ESR. The first febrile wave is followed by a period of apyrexia, lasting 7-14 days. The second feverish wave begins as acutely as the first, the temperature rises to high numbers. Patients are lethargic, inhibited, nausea and vomiting appear, and meningeal and focal symptoms of damage to the nervous system are detected. In peripheral blood - leukocytosis. This is a qualitatively new phase of the disease; it is always more severe than the first and lasts longer. During the first feverish wave, normal cytosis and increased cerebrospinal fluid pressure are detected in the cerebrospinal fluid. During the second wave, cytosis is 100-200 or more cells per 1 μl, lymphocytes predominate. The protein and sugar content increases. The course of the disease is acute, recovery is complete. There are isolated cases of chronic progressive course.
Complications and damage to the nervous system. With all the above-described clinical forms of tick-borne encephalitis, epileptiform, hyperkinetic syndromes and some other signs of damage to the nervous system can be observed. This depends on the epidemic focus (western, eastern), on the method of infection (vector-borne, nutritional), on the condition of the person at the time of infection and on the methods of therapy.
Hyperkinetic syndrome is registered relatively often (in 1/4 of patients), and mainly in persons under 16 years of age. The syndrome is characterized by the appearance of spontaneous rhythmic contractions (myoclonus) in individual muscle groups of paretic limbs already in the acute period of the disease.
Progressive forms. From the moment of infection and subsequently, even after the acute period, the tick-borne encephalitis virus can persist in the central nervous system in an active form. In these cases infectious process does not end, but goes into the phase of chronic (progressive) infection. Chronic infection with tick-borne encephalitis can occur in latent form and manifest themselves after several months and years under the influence of provoking factors (physical and mental trauma, early spa and physiotherapeutic treatment, abortion, etc.). The following types of progressive course are possible: primary and secondary progressive, and subacute course.
Diagnosis of Tick-borne encephalitis
In the diagnosis of tick-borne encephalitis great importance have anamnestic data: stay in an endemic focus, the patient’s profession, illness in the spring-summer period, tick bite. However, not every disease that occurs after such a bite is encephalitis. It is known that only 0.5-5% of all ticks are carriers of viruses. Accurate diagnosis of the disease is possible with the help of RSK, RN and RTGA. Isolation of the virus from the blood and cerebrospinal fluid has a certain diagnostic value. RSC gives a positive result from the 2nd week of the disease, RN - from the 8-9th week. It is also important to detect an increase in the titer of antiviral antibodies at the 3-4th week of the disease. Immunity after tick-borne encephalitis is persistent, virus-neutralizing antibodies are detected in the blood for many years. Leukocytosis and an increase in ESR are observed in the blood. In the cerebrospinal fluid - an increase in protein up to 1 g/l, lymphocytic pleocytosis.
Tick-borne encephalitis should be differentiated from various forms serous meningitis, typhus, Japanese mosquito encephalitis (in the Far East), acute polio. Differential diagnosis with the latter in children it can present significant difficulties, especially with the polio form of encephalitis. You should pay attention to the localization of the process, which in encephalitis corresponds to the cervical segments of the spinal cord (this is due to the perineural spread of the virus with a frequent bite in the neck), and in polio - to the lumbar segments (the virus multiplies in the intestines) with the corresponding localization of paresis. With tick-borne encephalitis, the “mosaic” clinical symptoms typical of polio are absent.
Treatment of tick-borne encephalitis
There is no etiotropic treatment yet. And in the first days of the disease, 3-6 ml of anti-tick γ-globulin or the serum of those who have recovered from tick-borne encephalitis, specific immunoglobulin IV, the immunoregulatory protein interferon-α, and the antiviral drug ribavirin are administered. However, some researchers consider such treatment to be ineffective, believing that the main role in pathogenesis is played not by humoral, but cellular immunity and by the time treatment is needed, the patient’s blood already contains high level antibodies. It has not yet been possible to conduct randomized, double-blind, placebo-controlled studies in acute neuroinfections. Prescribe detoxification therapy, medications that maintain water and electrolyte balance, and, if necessary, dehydration and other symptomatic medications.
Emergency care for tick-borne encephalitis. If symptoms of tick-borne encephalitis are detected, the patient should be urgently admitted to an infectious diseases hospital for intensive treatment.
Prevention of tick-borne encephalitis
Prevention of tick-borne encephalitis. Most effective protection against tick-borne encephalitis is vaccination. When visiting tick habitats, wear protective clothing and use repellent.
If a tick is sucked on, it should be removed; to be examined for infection with tick-borne encephalitis and other infections, you should go to an infectious diseases hospital. At positive result During the course of the study, the victim is given immunoglobulin against tick-borne encephalitis. Its administration is most effective within 1 day after a tick bite; it is not administered 4 days after a tick bite.
Use only boiled or pasteurized milk.
One of the latest achievements of science has been the creation of highly effective antiviral drug called yodantipyrine. Yodantipyrine is able to destroy the tick-borne encephalitis virus within 12-24 hours from the moment of infection (tick bite).
In the event of a child being bitten by a tick for the purpose of emergency prevention tick-borne encephalitis, it is recommended to use anaferon for children in doses: under the age of 12 years, 1 tablet 3 times a day, over the age of 12 years, 2 tablets 3 times a day for 21 days (incubation period of tick-borne encephalitis), which prevents the development of the disease.
Which doctors should you contact if you have tick-borne encephalitis?
Infectious disease specialist
Promotions and special offers
The Russian Ministry of Health has approved the drug Revolade (Eltrombopag) for use in children. New drug indicated for patients suffering from chronic immune thrombocytopenia (idiopathic thrombocytopenic purpura, ITP), rare disease blood systems.
Almost 5% of all malignant tumors constitute sarcomas. They are highly aggressive, rapidly spread hematogenously, and are prone to relapse after treatment. Some sarcomas develop for years without showing any signs...
Viruses not only float in the air, but can also land on handrails, seats and other surfaces, while remaining active. Therefore, when traveling or in public places It is advisable not only to exclude communication with other people, but also to avoid...
Return good vision and say goodbye to glasses forever contact lenses- the dream of many people. Now it can be made a reality quickly and safely. New opportunities laser correction vision is opened by the completely non-contact Femto-LASIK technique.
Cosmetics designed to care for our skin and hair may actually not be as safe as we think
Encephalitis caused by the ixodid tick is dangerous. Basic source of infection– tick saliva, which, when it enters human blood, causes vital damage important organs: brain (spinal cord), central nervous system. What are the different forms of encephalitis, how the virus affects the body, and for what symptoms you need to immediately consult a doctor, we will consider in more detail in this article.
Forms of tick-borne encephalitis
The disease develops in stages. First up 3-7 days When the virus enters the body, it is in the incubation stage. The infection is focal, the peak of the outbreak occurs in Aug. Sept month. It is during this period of the year that the tick is most active. With a decrease in immunity, the disease begins to rapidly progress, moving from one form to another.
There are 4 periods (forms) of encephalitis:
- Feverish, primary initial stage encephalitis. The symptoms are vivid, like the flu: fever, chills, fever, toxicosis, aching bones. After 8-10 days, the symptoms subside and become less pronounced. The patient, who has completed the course of treatment on time, begins to recover.
- Meningeal, replaces the primary febrile form. If the virus is not eliminated in a timely manner, it quickly penetrates the blood, affecting the nervous system and meninges. Symptoms appear in the form of headaches, vomiting, a sharp increase in temperature, and muscle stiffness in the occipital region.
- Encephalitic, leads to brain damage. In addition to the above symptoms, the patient has pronounced disorders of the psyche and consciousness; there may be convulsions and paralysis. The condition is critical and requires urgent hospitalization of the patient. Available death.
- Poliomyelitis, leads to damage to neurons in the spinal cord and muscle paralysis. The patient remains disabled, even if the doctors manage to save his life.
Incubation period of tick-borne encephalitis in humans
The duration of the incubation period is 8-30 days. Depending on the state of immunity, the number of days may vary slightly.
During this period, the virus enters the blood, damages healthy cells, mutates, spreads throughout all vital systems:
- liver transplantation;
- blood vessels, spleen;
- lymph nodes;
- spinal cord;
- cervical spine;
- soft tissue of the brain;
- cerebellum.
Tick-borne encephalitis is dangerous, leading to damage to the nervous and motor systems. Primary symptoms begin to appear already during the incubation period.
Symptoms
It is with the beginning of the incubation period that the primary symptoms of inflammation become pronounced.
It is not difficult for doctors to diagnose the disease:

As the virus progresses by approximately 8-10 day crashes the cardiovascular system. Signs appear bronchitis (cough, chills). Pneumonia may be suspected.
It is in children due to unstable weak immunity symptoms are most pronounced. The incubation period is not long. Quickly, through 10-12 days turns into a more severe meningeal form. The kids start complaining about headaches, nausea, vomiting, chills.
Signs of meningitis are present:
- high temperature;
- violations psyche;
- since morning dizziness;
- sharp pain in the head;
- in blood increased level ESR, leukocytes.
On 10-12 knocks acute manifestations encephalitis goes away and becomes more lethargic. The process proceeds rather sparingly, but primary signs of paralysis, atrophy of the neck muscles and upper limbs(hanging head and arms along the body due to lack of tendon reflexes). Disorders of activity become more pronounced heart and respiratory organs.
Signs
Clinically, tick-borne encephalitis can manifest itself in different ways:
- Spreading through the blood, paralyzes the muscles of the neck and limbs.
- In the upper and lower sections weakness is observed, weakened arms and legs drooping in lashes. The patient has a fever, chills, a feeling of weakness, fatigue, and aches throughout the body.
- Coverings of the skin and oral mucosa in the acute course of encephalitis they are hyperemic.
- It often occurs paralysis, numbness (numbness) of the limbs, a feeling of stunnedness, tinnitus.
The condition is serious. Coma, loss and confusion, and fever are possible. directly depend on the localization of tick suction.
Course and prognosis
Despite the severe course of the disease, primary latent phase when taking timely therapeutic measures forecast positive. The patient quickly recovers and recovers.
It is worth understanding that the further the virus spreads through the blood, the worse the situation becomes. Defeat meninges, joints inevitably leads to serious consequences. Often, patients consult a doctor with meningeal encephalitis when headaches, photophobia, nausea, vomiting, and dizziness are present.
The course of the disease is especially severe when meningoencephalitic form diseases when there is overexcitation of psychomotor skills, hallucinations, and epileptic seizures.
At focal brain damage breathing is impaired, reflexes are asymmetrical and inhibited. Muscle muscles and facial expressions are susceptible to paralysis. Cerebellar subcortical syndrome is observed against the background epileptic seizures. Possible loss of consciousness, coma.
Prodromal syndrome present in the polio form of the disease. Spinal cord cells are irritated. There is numbness and weakness in the limbs. Clearly violated motor functions at the patient. The wave of fever in the first 3-4 days during the incubation period gives way to flaccid paresis in the neck, shoulders, and chest.
At this current illness, the head begins to hang on the chest, involuntarily throws back along with the arms. Posture becomes slouched and hunched. There are all the signs of polio leading to the end 2-3 weeks development of the disease to complete atrophy of muscles, then nerves and trunks.
If first 7 days wave of fever proceeds relatively easily and meningal symptoms are moderately expressed, then with the arrival of the second wave the temperature rises sharply, lethargy, lethargy and, most importantly, appear. damage to trunks, endings, cells of the nervous system. A new phase of the disease begins, the longest and most severe.
In the periphery of the blood, the number of lymphocytes, sugar and protein is exceeded. The course is progressing. As the nervous system is damaged, hyperkinetic or epileptic syndromes appear. Muscle groups are subject to paresis, heart contractions become spontaneous. The spread of infection to the brain complicates the course of the disease. The forecast becomes unfavorable.
If you don't take action Urgent measures Once the patient is hospitalized, the fatal outcome becomes obvious.
Diagnostics
First, the patient will be examined visually by the doctor, complaints will be heard, and information about the last places of stay where tick infection may have occurred will be heard. Next, the patient is redirected for testing if tick-borne encephalitis is suspected.
The set of diagnostic measures includes:
- carrying out PCR for the presence of antigens in the blood;
- take cerebrospinal fluid for analysis;
- examination ELISA reactions to antigen sensitivity;
- analysis blood composition for the presence of immunoglobulin.
Treatment
First of all, it is carried out detoxification of the body, at cardiovascular disorders – intensive care unit therapy.
Treatment of encephalitis– complex, by administering immunoglobulin injections in the first 3-4 days. It is important to prevent swelling from a tick bite in the head area.
In order to normalize blood circulation, improve the trophism of nerve tissues and fibers, it is prescribed antiviral therapy by administering interferon, intronamixin, and cycloferon as injections. When detoxifying the body, you cannot do without antipyretic, anti-inflammatory drugs.
To eliminate symptoms, medication treatment is indicated by prescribing:

Encephalitis- a complex infectious disease and the prescription of treatment, the choice of the correct tactics of the treatment regimen should only be dealt with by a competent specialist, an infectious disease doctor. The patient needs rest, inpatient treatment with the exclusion of all provoking stimuli.
Encephalitis is fraught with serious complications, so the treatment course is carried out under close supervision. under the supervision of a doctor the body's reaction to injected drugs. If there is no improvement, the doctor will select other means and methods of treatment to eliminate all unpleasant signs. Usually the course of treatment 3-5 days.
If there is no improvement, then urgent resuscitation methods of treatment are possible to eliminate the symptoms of the disease through the joint actions of doctors: infectious disease specialist, surgeon, therapist, cardiologist.
Self-medication,picking out tick and even more so cutting formed tumor on the head, in any other place is unacceptable. Incorrect treatment folk remedies in the form of poultices and lotions can only worsen the situation.
Patients are subject to urgent hospitalization if tick-borne encephalitis is suspected; they require bed rest and rest, and a gentle diet. Even after graduation treatment course the patient remains under the supervision of doctors. After 3-4 months it is subject to re-examination, and so on, possibly up to 3 years, until foci of infection, possible with encephalitis, are completely eliminated.
Encephalitis is a group inflammatory diseases brain substances that are infectious, allergic or toxic in nature. If a patient is diagnosed with a disease, he should be hospitalized immediately. In case of encephalitis, a person is placed in an infectious diseases or specialized neurological department and is prescribed strict bed rest and constant monitoring.
What is encephalitis
Encephalitis (lat. encephalitis - inflammation of the brain) is the name of a whole group of inflammatory processes that affect the human brain, appearing against the background of exposure to infectious pathogens and allergic agents, toxic substances.
Changes in nervous tissue during encephalitis are quite stereotypical, and only in some cases can signs be detected specific disease(rabies, for example). The significance for the body and the consequences of any inflammatory changes in the brain are always serious, so there is no need to once again remind us of their danger.
In the acute stage, it causes an inflammatory process in the brain substance, affecting the hypothalamus, basal ganglia, and nuclei of the oculomotor nerves. In the chronic stage, a toxic-degenerative process develops, most pronounced in the substantia nigra and globus pallidus.
The incubation period for encephalitis ranges from one to two weeks.
In case of encephalitis of any etiology, it is necessary complex therapy. As a rule, it includes etiotropic treatment (antiviral, antibacterial, antiallergic), dehydration, infusion therapy, anti-inflammatory treatment, vascular and neuroprotective therapy, and symptomatic treatment.
Classification
The classification of encephalitis reflects etiological factors related to them clinical manifestations and flow features.
Depending on the presence of inflammation of the meningeal membranes (linings of the brain), the following forms of encephalitis are distinguished:
- isolated - in the clinic there are symptoms only of encephalitis;
- meningoencephalitis - symptoms of inflammation of the meninges are also present in the clinic.
By localization:
- cortical;
- subcortical;
- stem;
- cerebellar damage.
According to the pace of development and flow:
- fast;
- spicy;
- subacute;
- chronic;
- recurrent.
By severity:
- moderate severity;
- heavy;
- extremely heavy.
Causes
Most often, encephalitis is caused by viruses - neuroinfections; sometimes it also occurs as complications of various infectious diseases.
A common cause of progression is neuroinfection. It is worth noting that the etiology of the disease directly depends on its type. Thus, the reasons for the progression of viral encephalitis are: the bite of infected insects (usually carried by mosquitoes or ticks), the penetration of influenza, herpes, and rabies viruses into the body.
Ways the virus enters the human body:
- insect bite (hematogenous route);
- with direct contact;
- nutritional route;
- airborne route.
Anyone can develop the disease, but older people and children are at greatest risk. Those who are also prone to the disease the immune system suppressed or weakened by some influence, for example during treatment for cancer, HIV infection or long-term use of steroids.
Symptoms of encephalitis
The disease usually begins with fever and headache, then the symptoms increase sharply and worsen - convulsions (fits), confusion and loss of consciousness, drowsiness and even coma are observed. Encephalitis can be seriously life-threatening.
Symptoms of encephalitis depend on many factors: the causative agent of the disease, its pathology, course and location.
The disease in many situations manifests itself as aches and pain. At the same time, these unpleasant symptoms affect the whole body: joints, muscles.
However, there are symptoms common to all types of encephalitis:
- headache - it is most often expressed in all areas of the head (diffuse), can be pressing, bursting;
- nausea and vomiting that does not bring relief;
- torticollis, tremor, seizures;
- The main symptom of encephalitis is sudden jump temperatures up to high values(39–40°C);
- oculomotor disorders: ptosis (drooping of the upper eyelid), diplopia (double vision), ophthalmoplegia (lack of eyeball movements);
- Rarely, damage to the facial nerve is possible with the development of paresis of facial muscles, the trigeminal nerve with pain in the face, and isolated convulsions are possible.
Depending on the type of pathogen, the time interval between infection and the appearance of the first symptoms lasts from 7 to 20 days. During the latent period, the infection does not reveal itself; the presence of the pathogen can only be detected in a laboratory setting.
Other possible signs of encephalitis:
- increased muscle tone;
- involuntary movements (hyperkinesis);
- strabismus, impaired movements of the eyeballs (ophthalmoparesis);
- diplopia (double vision);
- ptosis (drooping) of the upper eyelid;
Another characteristic feature- These are muscle twitches in humans. These twitches occur involuntarily. It is important to note that sometimes a person is bothered by numbness of the skin, which manifests itself in different parts bodies.
Types of encephalitis
Despite all the variety of causes and types, its manifestations are quite stereotypical when severe course disease, but if inflammation of the nervous tissue accompanies other ailments, then recognizing encephalitis as such is not so easy.
Epidemic encephalitis Economo(lethargic encephalitis A)
The causative agent is a filterable virus that has not been isolated to date. This type of virus is transmitted by airborne droplets.
Signs of developing epidemic encephalitis:
- temperature rise to 38-39 degrees;
- chills;
- increased drowsiness;
- fatigue;
- lack of appetite;
- headache.
IN in this case urgent hospitalization is required. The exact duration of the incubation period is unknown, so all those in contact with a sick person should be monitored for three months.
Tick-borne encephalitis
Therefore, you should not neglect vaccination (vaccination) against certain types encephalitis when traveling to areas with unfavorable conditions for this disease.
All encephalitis is treated in infectious diseases hospitals. In the chronic stage, it is necessary to regularly visit a neurologist, as well as take courses of medications aimed at improving brain activity and restoring ataxic and motor defects.
Prevention
Preventative measures taken to prevent different types encephalitis, differ and are represented by the following events:
- Preventive measures that can, if possible, prevent infection with tick-borne and mosquito-borne encephalitis are preventive vaccination people living and/or working in the zones possible infection. Standard vaccination against tick-borne encephalitis includes 3 vaccinations and provides lasting immunity for 3 years.
- Prevention of secondary encephalitis involves timely diagnosis And adequate therapy infectious diseases.
- Limiting tourist travel to countries where infection with viral encephalitis through mosquito bites is possible.

