Thank you
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
Adrenergic blockers are a group of drugs united by a common pharmacological action - the ability to neutralize adrenaline receptors of blood vessels and the heart. That is, adrenergic blockers “turn off” the receptors that normally respond to adrenaline and norepinephrine. Accordingly, the effects of adrenergic blockers are completely opposite to those of adrenaline and norepinephrine.general characteristics
Adrenergic blockers act on adrenergic receptors, which are located in the walls of blood vessels and in the heart. Actually, this group of drugs got their name precisely from the fact that they block the action of adrenergic receptors.Normally, when adrenergic receptors are free, they can be affected by adrenaline or norepinephrine that appears in the bloodstream. Adrenaline, when bound to adrenergic receptors, provokes the following effects:
- Vasoconstrictor (the lumen of blood vessels sharply narrows);
- Hypertensive (blood pressure increases);
- Antiallergic;
- Bronchodilator (expands the lumen of the bronchi);
- Hyperglycemic (increases blood glucose levels).
Classification
There are four types of adrenergic receptors in the walls of blood vessels - alpha-1, alpha-2, beta-1 and beta-2, which are usually called respectively: alpha-1-adrenergic receptors, alpha-2-adrenergic receptors, beta-1-adrenergic receptors and beta -2-adrenergic receptors. Drugs from the adrenergic blocking group can turn off various types of receptors, for example, only beta-1 adrenergic receptors or alpha-1,2 adrenergic receptors, etc. Adrenergic blockers are divided into several groups depending on which types of adrenergic receptors they turn off.So, adrenergic blockers are classified into the following groups:
1. Alpha blockers:
- Alpha-1 blockers (alfuzosin, doxazosin, prazosin, silodosin, tamsulosin, terazosin, urapidil);
- Alpha-2 blockers (yohimbine);
- Alpha-1,2-adrenergic blockers (nicergoline, phentolamine, proroxan, dihydroergotamine, dihydroergocristine, alpha-dihydroergocriptine, dihydroergotoxin).
- Beta-1,2-blockers (also called non-selective) - bopindolol, metypranolol, nadolol, oxprenolol, pindolol, propranolol, sotalol, timolol;
- Beta-1 blockers (also called cardioselective or simply selective) - atenolol, acebutolol, betaxolol, bisoprolol, metoprolol, nebivolol, talinolol, celiprolol, esatenolol, esmolol.
This classification provides the international names of the active substances included in the composition of drugs belonging to each group of adrenergic blockers.
Each group of beta-blockers is also divided into two types - with intrinsic sympathomimetic activity (ISA) or without ISA. However, this classification is auxiliary and is necessary only for doctors to select the optimal drug.
Adrenergic blockers - list
We present lists of drugs for each group of adrenergic blockers (alpha and beta) separately to avoid confusion. In all lists, we first indicate the name of the active substance (INN), and then below - the commercial names of the drugs that contain this active ingredient.Alpha adrenergic blocking drugs
We present lists of alpha-blockers of various subgroups in different lists for the easiest and most structured search for the necessary information. To drugs of the alpha-1-adrenergic blocking group include the following:
To drugs of the alpha-1-adrenergic blocking group include the following:
1. Alfuzosin (INN):
- Alfuprost MR;
- Alfuzosin;
- Alfuzosin hydrochloride;
- Dalfaz;
- Dalfaz Retard;
- Dalfaz SR.
- Artesin;
- Artesin Retard;
- Doxazosin;
- Doxazosin Belupo;
- Doxazosin Zentiva;
- Doxazosin Sandoz;
- Doxazosin-ratiopharm;
- Doxazosin Teva;
- Doxazosin mesylate;
- Zoxon;
- Kamiren;
- Kamiren HL;
- Cardura;
- Cardura Neo;
- Tonocardin;
- Urocard.
- Polpressin;
- Prazosin.
- Urorek.
- Hypersimple;
- Glansin;
- Miktosin;
- Omnic Okas;
- Omnic;
- Omsulosin;
- Proflosin;
- Sonizin;
- Tamzelin;
- Tamsulosin;
- Tamsulosin Retard;
- Tamsulosin Sandoz;
- Tamsulosin-OBL;
- Tamsulosin Teva;
- Tamsulosin hydrochloride;
- Tamsulon FS;
- Taniz ERAS;
- Taniz K;
- Tulosin;
- Focusin.
- Cornam;
- Setegis;
- Terazosin;
- Terazosin Teva;
- Haytrin.
- Urapidil Karino;
- Ebrantil.
To drugs of the alpha-1,2-adrenergic blocking group The following drugs include:
1. Dihydroergotoxin (a mixture of dihydroergotamine, dihydroergocristine and alpha-dihydroergocriptine):
- Redergin.
- Ditamin.
- Nilogrin;
- Nicergoline;
- Nicergolin-Verein;
- Sermion.
- Pyrroxane;
- Proroksan.
- Phentolamine.
Beta blockers - list
 Since each group of beta-blockers includes a fairly large number of drugs, we present their lists separately for easier comprehension and search for the necessary information.
Since each group of beta-blockers includes a fairly large number of drugs, we present their lists separately for easier comprehension and search for the necessary information. Selective beta blockers (beta-1 blockers, selective blockers, cardioselective blockers). The generally accepted names of this pharmacological group of adrenergic blockers are listed in parentheses.
So, selective beta-blockers include the following drugs:
1. Atenolol:
- Atenobene;
- Atenova;
- Atenol;
- Atenolan;
- Atenolol;
- Atenolol-Agio;
- Atenolol-AKOS;
- Atenolol-Acri;
- Atenolol Belupo;
- Atenolol Nycomed;
- Atenolol-ratiopharm;
- Atenolol Teva;
- Atenolol UBF;
- Atenolol FPO;
- Atenolol Stada;
- Atenosan;
- Betacard;
- Velorin 100;
- Vero-Atenolol;
- Ormidol;
- Prinorm;
- Sinar;
- Tenormin.
- Acekor;
- Sectral.
- Betak;
- Betaxolol;
- Betalmik EU;
- Betoptik;
- Betoptik S;
- Betoftan;
- Xonephus;
- Xonef BC;
- Lokren;
- Optibetol.
- Aritel;
- Aritel Core;
- Bidop;
- Bidop Cor;
- Biol;
- Biprol;
- Bisogamma;
- Bisocard;
- Bisomore;
- Bisoprolol;
- Bisoprolol-OBL;
- Bisoprolol LEKSVM;
- Bisoprolol Lugal;
- Bisoprolol Prana;
- Bisoprolol-ratiopharm;
- Bisoprolol C3;
- Bisoprolol Teva;
- Bisoprolol fumarate;
- Concor Cor;
- Corbis;
- Cordinorm;
- Cordinorm Cor;
- Coronal;
- Niperten;
- Tirez.
- Betalok;
- Betalok ZOK;
- Vasocordin;
- Corvitol 50 and Corvitol 100;
- Metozok;
- Metocard;
- Metokor Adifarm;
- Metolol;
- Metoprolol;
- Metoprolol Acri;
- Metoprolol Akrikhin;
- Metoprolol Zentiva;
- Metoprolol Organic;
- Metoprolol OBL;
- Metoprolol-ratiopharm;
- Metoprolol succinate;
- Metoprolol tartrate;
- Serdol;
- Egilok Retard;
- Egilok S;
- Emzok.
- Bivotens;
- Binelol;
- Nebivator;
- Nebivolol;
- Nebivolol NANOLEK;
- Nebivolol Sandoz;
- Nebivolol Teva;
- Nebivolol Chaikapharma;
- Nebivolol STADA;
- Nebivolol hydrochloride;
- Nebikor Adifarm;
- Nebilan Lannacher;
- Nebilet;
- Nebilong;
- OD-Sky.
7.
Talinolol:
- Cordanum.
- Celiprol.
- Estekor.
- Breviblock.
1. Bopindolol:
- Sandorm.
- Trimepranol.
- Korgard.
- Trazikor.
- Whisken.
- Anaprilin;
- Vero-Anaprilin;
- Inderal;
- Inderal LA;
- Obzidan;
- Propranobene;
- Propranolol;
- Propranolol Nycomed.
- Darob;
- SotaHEXAL;
- Sotalex;
- Sotalol;
- Sotalol Canon;
- Sotalol hydrochloride.
- Arutimol;
- Glaumol;
- Glautam;
- Cusimolol;
- Niolol;
- Okumed;
- Okumol;
- Okupres E;
- Optimol;
- Oftan Timogel;
- Oftan Timolol;
- Oftensin;
- ThymoHEXAL;
- Thymol;
- Timolol;
- Timolol AKOS;
- Timolol Betalec;
- Timolol Bufus;
- Timolol DIA;
- Timolol LENS;
- Timolol MEZ;
- Timolol POS;
- Timolol Teva;
- Timolol maleate;
- Timollong;
- Timoptic;
- Timoptic depot.
Alpha-beta adrenergic blockers (drugs that turn off both alpha and beta adrenergic receptors)
 Drugs in this group include the following:
Drugs in this group include the following: 1. Butylmethyloxadiazole:
- Albetor;
- Albetor Long;
- Butylmethyloxadiazole;
- Proxodolol.
- Acridilol;
- Bagodilol;
- Vedicardol;
- Dilatrend;
- Karvedigamma;
- Carvedilol;
- Carvedilol Zentiva;
- Carvedilol Canon;
- Carvedilol Obolenskoe;
- Carvedilol Sandoz;
- Carvedilol Teva;
- Carvedilol STADA;
- Carvedilol-OBL;
- Carvedilol Pharmaplant;
- Carvenal;
- Carvetrend;
- Carvidil;
- Cardivas;
- Coriol;
- Credex;
- Recardium;
- Talliton.
- Abetol;
- Amipress;
- Labetol;
- Trandol.
Beta-2 blockers
There are currently no drugs that specifically turn off only beta-2 adrenergic receptors. Previously, the drug Butoxamine, which is a beta-2 adrenergic blocker, was produced, but today it is not used in medical practice and is of interest exclusively to experimental scientists specializing in the field of pharmacology, organic synthesis, etc.There are only non-selective beta-blockers that simultaneously turn off both beta-1 and beta-2 adrenergic receptors. However, since there are also selective adrenergic blockers that turn off exclusively beta-1 adrenergic receptors, non-selective ones are often called beta-2 adrenergic blockers. This name is incorrect, but quite widespread in everyday life. Therefore, when they say “beta-2-blockers,” you need to know that they mean a group of non-selective beta-1,2-blockers.
Action
Since turning off various types of adrenergic receptors leads to the development of generally common, but different in some aspects, effects, we will consider the action of each type of adrenergic blockers separately.Action of alpha-blockers
Alpha-1-blockers and alpha-1,2-blockers have the same pharmacological effects. And the drugs of these groups differ from each other in side effects, of which alpha-1,2-adrenergic blockers usually have more, and they occur more often compared to alpha-1-adrenergic blockers.Thus, drugs from these groups dilate blood vessels in all organs, and especially strongly in the skin, mucous membranes, intestines and kidneys. Due to this, the total peripheral vascular resistance decreases, blood flow and blood supply to peripheral tissues improves, and blood pressure decreases. By reducing peripheral vascular resistance and reducing the amount of blood that returns to the atria from the veins (venous return), the pre- and afterload on the heart is significantly reduced, which significantly facilitates its work and has a positive effect on the condition of this organ. Summarizing the above, we can conclude that alpha-1-blockers and alpha-1,2-blockers have the following effects:
- Reduce blood pressure, reduce total peripheral vascular resistance and afterload on the heart;
- Dilate small veins and reduce preload on the heart;
- Improves blood circulation both throughout the body and in the heart muscle;
- Improve the condition of people suffering from chronic heart failure, reducing the severity of symptoms (shortness of breath, pressure surges, etc.);
- Reduce pressure in the pulmonary circulation;
- Reduce the level of total cholesterol and low-density lipoproteins (LDL), but increase the content of high-density lipoproteins (HDL);
- Increases cell sensitivity to insulin, due to which glucose is used faster and more efficiently, and its concentration in the blood decreases.
In addition, alpha-blockers reduce the severity of symptoms of inflammatory and obstructive processes in the genitourinary organs caused by prostatic hyperplasia. That is, the drugs eliminate or reduce the severity of incomplete emptying of the bladder, night urination, frequent urination and burning during urination.
Alpha-2 adrenergic blockers have little effect on the blood vessels of internal organs, including the heart; they primarily affect the vascular system of the genital organs. That is why alpha-2 adrenergic blockers have a very narrow scope of application - the treatment of impotence in men.
Action of non-selective beta-1,2-blockers

- Reduce heart rate;
- Reduce blood pressure and moderately reduce total peripheral vascular resistance;
- Reduce myocardial contractility;
- Reduce the oxygen demand of the heart muscle and increase the resistance of its cells to oxygen starvation (ischemia);
- Reduce the degree of activity of excitation foci in the conduction system of the heart and, thereby, prevent arrhythmias;
- Reduce the production of renin by the kidneys, which also leads to a decrease in blood pressure;
- At the initial stages of use, the tone of blood vessels increases, but then it decreases to normal or even lower;
- Prevent platelet aggregation and blood clot formation;
- Improve the delivery of oxygen from red blood cells to the cells of organs and tissues;
- Strengthens contractions of the myometrium (muscular layer of the uterus);
- Increases the tone of the bronchi and esophageal sphincter;
- Strengthen the motility of the digestive tract;
- Relaxes the bladder detrusor;
- Slow down the formation of active forms of thyroid hormones in peripheral tissues (only some beta-1,2-blockers).
In women, non-selective beta blockers increase uterine contractility and reduce blood loss during childbirth or after surgery.
In addition, due to their effect on the vessels of peripheral organs, non-selective beta blockers reduce intraocular pressure and reduce the production of moisture in the anterior chamber of the eye. This effect of drugs is used in the treatment of glaucoma and other eye diseases.
The effect of selective (cardioselective) beta-1 blockers
Drugs in this group have the following pharmacological effects:- Reduce heart rate (HR);
- Reduce the automaticity of the sinus node (pacemaker);
- They inhibit the conduction of impulses through the atrioventricular node;
- Reduce contractility and excitability of the heart muscle;
- Reduces the heart's need for oxygen;
- Suppress the effects of adrenaline and norepinephrine on the heart under conditions of physical, mental or emotional stress;
- Reduce blood pressure;
- Normalizes heart rhythm during arrhythmias;
- Limit and prevent the spread of the damage zone during myocardial infarction.
In addition, beta-1 blockers eliminate arrhythmia and narrowing of the lumen of small vessels. In people suffering from bronchial asthma, they reduce the risk of bronchospasm, and in people with diabetes, they reduce the likelihood of developing hypoglycemia (low blood sugar).
Action of alpha-beta blockers
 Drugs in this group have the following pharmacological effects:
Drugs in this group have the following pharmacological effects: - Reduce blood pressure and reduce total peripheral vascular resistance;
- Reduce intraocular pressure in open-angle glaucoma;
- Normalize lipid profile parameters (reduce the level of total cholesterol, triglycerides and low-density lipoproteins, but increase the concentration of high-density lipoproteins).
In addition, alpha-beta blockers improve myocardial contractility, due to which the blood does not remain in the left ventricle after contraction, but is completely thrown into the aorta. This helps to reduce the size of the heart and reduces the degree of its deformation. By improving heart function, drugs in this group for congestive heart failure increase the severity and volume of tolerated physical, mental and emotional stress, reduce the frequency of heart contractions and attacks of coronary artery disease, and also normalize the cardiac index.
The use of alpha-beta blockers reduces mortality and the risk of recurrent heart attack in people with coronary artery disease or dilated cardiomyopathy.
Application
Let us consider the indications and scope of application of various groups of adrenergic blockers separately in order to avoid confusion.Indications for the use of alpha-blockers
Since drugs from subgroups of alpha-blockers (alpha-1, alpha-2 and alpha-1,2) have different mechanisms of action and are somewhat different from each other in the nuances of their effect on blood vessels, their scope of application and, accordingly, indications are also different.Alpha-1 blockers indicated for use in the following conditions and diseases:
- Hypertension (to reduce blood pressure);
- Benign prostatic hyperplasia.
- Peripheral circulation disorders (for example, Raynaud's disease, endarteritis, etc.);
- Dementia (dementia) caused by the vascular component;
- Vertigo and disturbances of the vestibular apparatus caused by vascular factors;
- Diabetic angiopathy;
- Dystrophic diseases of the cornea;
- Optic neuropathy caused by ischemia (oxygen starvation);
- Prostate hypertrophy;
- Urinary disorders due to a neurogenic bladder.
Use of beta-blockers (indications)
Selective and non-selective beta-blockers have slightly different indications and areas of application, which is due to differences in certain nuances of their effect on the heart and blood vessels.Indications for the use of non-selective beta-1,2-blockers the following:
- Arterial hypertension ;
- Angina pectoris;
- Sinus tachycardia;
- Prevention of ventricular and supraventricular arrhythmias, as well as bigeminy, trigeminy;
- Mitral valve prolapse;
- Myocardial infarction;
- Migraine prevention;
- Increased intraocular pressure.
Cardioselective beta-1 blockers are indicated for use if a person has the following diseases or conditions:
- Arterial hypertension of moderate or low severity;
- Cardiac ischemia;
- Hyperkinetic cardiac syndrome;
- Various types of arrhythmias (sinus, paroxysmal, supraventricular tachycardia, extrasystole, atrial flutter or fibrillation, atrial tachycardia);
- Hypertrophic cardiomyopathy;
- Mitral valve prolapse;
- Myocardial infarction (treatment of an existing heart attack and prevention of a recurrence);
- Migraine prevention;
- Neurocirculatory dystonia of the hypertensive type;
- In the complex therapy of pheochromocytoma, thyrotoxicosis and tremor;
- Akathisia caused by taking antipsychotics.
Indications for the use of alpha-beta blockers
Drugs in this group are indicated for use if a person has the following conditions or diseases:- Arterial hypertension;
- Stable angina;
- Chronic heart failure (as part of combination therapy);
- Arrhythmia;
- Glaucoma (the drug is administered as eye drops).
Side effects
Let's consider the side effects of adrenergic blockers of different groups separately, since, despite the similarities, there are a number of differences between them.All alpha-blockers can provoke both the same and different side effects, which is due to the peculiarities of their effect on certain types of adrenergic receptors.
Side effects of alpha blockers
 So, all alpha blockers (alpha 1, alpha 2 and alpha 1,2)
provoke the following identical side effects:
So, all alpha blockers (alpha 1, alpha 2 and alpha 1,2)
provoke the following identical side effects: - Headache;
- Orthostatic hypotension (a sharp decrease in blood pressure when moving to a standing position from a sitting or lying position);
- Syncope (short-term fainting);
- Nausea or vomiting;
- Constipation or diarrhea.
- Hypotension (severe decrease in blood pressure);
- Tachycardia (palpitations);
- Arrhythmia;
- Dyspnea;
- Blurred vision (fog before the eyes);
- Xerostomia;
- Feeling of discomfort in the abdomen;
- Cerebrovascular accidents;
- Decreased libido;
- Priapism (prolonged painful erections);
- Allergic reactions (rash, skin itching, urticaria, Quincke's edema).
- Excitement;
- Coldness of the extremities;
- Angina attack;
- Increased acidity of gastric juice;
- Ejaculation disorders;
- Pain in the limbs;
- Allergic reactions (redness and itching of the upper half of the body, urticaria, erythema).
- Tremor;
- Excitation;
- Irritability;
- Increased blood pressure;
- Tachycardia;
- Increased motor activity;
- Abdominal pain;
- Priapism;
- Decreased frequency and quantity of urination.
Beta blockers - side effects
Selective (beta-1) and non-selective (beta-1,2) adrenergic blockers have both the same side effects and different ones, which is due to the peculiarities of their effect on different types of receptors.So, The following side effects are the same for selective and non-selective beta-blockers:
- Dizziness;
- Headache;
- Drowsiness;
- Insomnia;
- Nightmarish dreams;
- Fatigue;
- Weakness;
- Anxiety;
- Confusion;
- Brief episodes of memory loss;
- Slow response;
- Paresthesia (feeling of goose bumps, numbness of the limbs);
- Impaired vision and taste;
- Dry mouth and eyes;
- Bradycardia;
- Heartbeat;
- Atrioventricular block;
- Conduction disturbances in the heart muscle;
- Arrhythmia;
- Deterioration of myocardial contractility;
- Hypotension (low blood pressure);
- Heart failure;
- Raynaud's phenomenon;
- Pain in the chest, muscles and joints;
- Thrombocytopenia (a decrease in the total number of platelets in the blood below normal);
- Agranulocytosis (absence of neutrophils, eosinophils and basophils in the blood);
- Nausea and vomiting;
- Abdominal pain;
- Diarrhea or constipation;
- Liver disorders;
- Dyspnea;
- Spasm of the bronchi or larynx;
- Allergic reactions (skin itching, rash, redness);
- Sweating;
- Coldness of the extremities;
- Muscle weakness;
- Decreased libido;
- Increase or decrease in enzyme activity, bilirubin and glucose levels in the blood.
 Non-selective beta-blockers (beta-1,2), in addition to those listed above, can also provoke the following side effects:
Non-selective beta-blockers (beta-1,2), in addition to those listed above, can also provoke the following side effects:
- Eye irritation;
- Diplopia (double vision);
- Nasal congestion;
- Respiratory failure;
- Collapse;
- Exacerbation of intermittent claudication;
- Temporary disturbances of cerebral circulation;
- Cerebral ischemia;
- Fainting;
- Decreased hemoglobin levels in the blood and hematocrit;
- Quincke's edema;
- Change in body weight;
- Lupus syndrome;
- Impotence;
- Peyronie's disease;
- Thrombosis of the intestinal mesenteric artery;
- Colitis;
- Increased levels of potassium, uric acid and triglycerides in the blood;
- Blurred and decreased visual acuity, burning, itching and foreign body sensation in the eyes, lacrimation, photophobia, corneal edema, inflammation of the eyelid margins, keratitis, blepharitis and keratopathy (for eye drops only).
Side effects of alpha-beta blockers
Side effects of alpha-beta blockers include some of the side effects of both alpha and beta blockers. However, they are not identical to the side effects of alpha blockers and beta blockers, since the set of symptoms of the side effects is completely different. So, Alpha-beta blockers have the following side effects:- Dizziness;
- Headache;
- Asthenia (feeling of fatigue, loss of strength, indifference, etc.);
- Syncope (short-term fainting);
- Muscle weakness;
- General weakness and fatigue;
- Sleep disorders;
- Depression;
- Paresthesia (feeling of goosebumps, numbness of the limbs, etc.);
- Xerophthalmia (dry eye);
- Decreased production of tear fluid;
- Bradycardia;
- Violation of atrioventricular conduction up to blockade;
- Postural hypotension;
- Pain in the chest, abdomen and limbs;
- Angina;
- Deterioration of peripheral circulation;
- Worsening of the course of heart failure;
- Exacerbation of Raynaud's syndrome;
- Edema;
- Thrombocytopenia (a decrease in the number of platelets in the blood below normal);
- Leukopenia (decreased total number;
- Coldness of the extremities;
- Block of the Hiss bundle branches.
- Bradycardia;
- Reduced blood pressure;
- Bronchospasm;
- Dizziness;
- Weakness;
- Sensation of burning or foreign body in the eye;
Contraindications
Contraindications to the use of various groups of alpha-blockers
Contraindications to the use of various groups of alpha-blockers are given in the table.| Contraindications to the use of alpha-1-blockers | Contraindications to the use of alpha-1,2-blockers | Contraindications to the use of alpha-2 blockers |
| Stenosis (narrowing) of the aortic or mitral valves | Severe peripheral vascular atherosclerosis | |
| Orthostatic hypotension | Arterial hypotension | Blood pressure surges |
| Severe liver dysfunction | Hypersensitivity to drug components | Uncontrolled hypotension or hypertension |
| Pregnancy | Angina pectoris | Severe liver or kidney problems |
| Lactation | Bradycardia | |
| Hypersensitivity to drug components | Organic heart lesions | |
| Heart failure secondary to constrictive pericarditis or cardiac tamponade | Myocardial infarction less than 3 months ago | |
| Heart defects occurring against the background of low filling pressure of the left ventricle | Acute bleeding | |
| Severe renal failure | Pregnancy | |
| Lactation |
Beta blockers - contraindications
Selective (beta-1) and non-selective (beta-1,2) adrenergic blockers have almost identical contraindications for use. However, the range of contraindications to the use of selective beta blockers is somewhat wider than for non-selective ones. All contraindications for use for beta-1- and beta-1,2-blockers are reflected in the table.| Contraindications to the use of non-selective (beta-1,2) adrenergic blockers | Contraindications to the use of selective (beta-1) adrenergic blockers |
| Individual hypersensitivity to drug components | |
| Atrioventricular block II or III degree | |
| Sinoatrial blockade | |
| Severe bradycardia (pulse less than 55 beats per minute) | |
| Sick sinus syndrome | |
| Cardiogenic shock | |
| Hypotension (systolic pressure value below 100 mm Hg. Art.) | |
| Acute heart failure | |
| Chronic heart failure in the stage of decompensation | |
| Obliterating vascular diseases | Peripheral circulation disorders |
| Prinzmetal's angina | Pregnancy |
| Bronchial asthma | Lactation |
Contraindications to the use of alpha-beta blockers
Contraindications to the use of alpha-beta blockers are as follows:- Increased individual sensitivity to any components of the drugs;
- Atrioventricular block II or III degree;
- Sinoatrial block;
- Sick sinus syndrome;
- Chronic heart failure in the decompensation stage (NYHA functional class IV);
- Cardiogenic shock;
- Sinus bradycardia (pulse less than 50 beats per minute);
- Arterial hypotension (systolic pressure below 85 mm Hg);
- Chronic obstructive pulmonary diseases;
- Bronchial asthma;
- Peptic ulcer of the stomach or duodenum;
- Diabetes mellitus type 1;
- Pregnancy and breastfeeding period;
- Severe liver diseases.
Antihypertensive beta-blockers
 Drugs of various groups of adrenergic blockers have a hypotensive effect. The most pronounced hypotensive effect is exerted by alpha-1-blockers containing substances such as doxazosin, prazosin, urapidil or terazosin as active ingredients. Therefore, it is the drugs of this group that are used for long-term therapy of hypertension in order to reduce blood pressure and subsequently maintain it at an average acceptable level. Drugs of the alpha-1-blocker group are optimal for use in people suffering only from hypertension, without concomitant cardiac pathology.
Drugs of various groups of adrenergic blockers have a hypotensive effect. The most pronounced hypotensive effect is exerted by alpha-1-blockers containing substances such as doxazosin, prazosin, urapidil or terazosin as active ingredients. Therefore, it is the drugs of this group that are used for long-term therapy of hypertension in order to reduce blood pressure and subsequently maintain it at an average acceptable level. Drugs of the alpha-1-blocker group are optimal for use in people suffering only from hypertension, without concomitant cardiac pathology. In addition, all beta-blockers are hypotensive - both selective and non-selective. Antihypertensive non-selective beta-1,2-adrenergic blockers containing bopindolol, metypranolol, nadolol, oxprenolol, pindolol, propranolol, sotalol, timolol as active substances. These drugs, in addition to the hypotensive effect, also affect the heart, so they are used not only in the treatment of arterial hypertension, but also heart diseases. The weakest antihypertensive non-selective beta blocker is sotalol, which has a predominant effect on the heart. However, this drug is used in the treatment of arterial hypertension, which is combined with heart disease. All non-selective beta blockers are optimal for use in hypertension combined with coronary artery disease, angina pectoris and previous myocardial infarction.
Antihypertensive selective beta-1-blockers are drugs containing the following active substances: atenolol, acebutolol, betaxolol, bisoprolol, metoprolol, nebivolol, talinolol, celiprolol, esatenolol, esmolol. Considering the characteristics of their action, these drugs are best suited for the treatment of arterial hypertension combined with obstructive pulmonary pathologies, peripheral arterial diseases, diabetes mellitus, atherogenic dyslipidemia, as well as for heavy smokers.
Alpha-beta blockers containing carvedilol or butylmethyloxadiazole as active substances are also hypotensive. But due to the wide range of side effects and pronounced effects on small vessels, drugs in this group are used less frequently compared to alpha-1 blockers and beta blockers.
Currently, beta-blockers and alpha-1 blockers are the drugs of choice for the treatment of hypertension.
Alpha-1,2-blockers are used mainly to treat disorders of peripheral and cerebral circulation, since they have a more pronounced effect on small blood vessels. Theoretically, drugs in this group can be used to lower blood pressure, but this is ineffective due to the large number of side effects that will occur.
Adrenergic blockers for prostatitis
 For prostatitis, alpha-1-blockers containing alfuzosin, silodosin, tamsulosin or terazosin as active substances are used to improve and facilitate the process of urination. Indications for the prescription of adrenergic blockers for prostatitis are low pressure inside the urethra, weak tone of the bladder itself or its neck, as well as the muscles of the prostate gland. The drugs normalize the flow of urine, which accelerates the elimination of decay products, as well as dead pathogenic bacteria and, accordingly, increases the effectiveness of antimicrobial and anti-inflammatory treatment. The positive effect usually fully develops after 2 weeks of use. Unfortunately, normalization of urine outflow under the influence of adrenergic blockers is observed only in 60–70% of men suffering from prostatitis.
For prostatitis, alpha-1-blockers containing alfuzosin, silodosin, tamsulosin or terazosin as active substances are used to improve and facilitate the process of urination. Indications for the prescription of adrenergic blockers for prostatitis are low pressure inside the urethra, weak tone of the bladder itself or its neck, as well as the muscles of the prostate gland. The drugs normalize the flow of urine, which accelerates the elimination of decay products, as well as dead pathogenic bacteria and, accordingly, increases the effectiveness of antimicrobial and anti-inflammatory treatment. The positive effect usually fully develops after 2 weeks of use. Unfortunately, normalization of urine outflow under the influence of adrenergic blockers is observed only in 60–70% of men suffering from prostatitis. The most popular and effective adrenergic blockers for prostatitis are drugs containing tamsulosin (for example, Hyperprost, Glansin, Mictosin, Omsulosin, Tulosin, Fokusin, etc.).
BBs are a group of pharmacological drugs, when introduced into the human body, blocking beta-adrenergic receptors.
Beta adrenergic receptors are divided into three subtypes:
beta1-adrenergic receptors, which are located in the heart and through which the stimulating effects of catecholamines on the activity of the heart pump are mediated: increased sinus rhythm, improved intracardiac conduction, increased myocardial excitability, increased myocardial contractility (positive chrono-, dromo-, batmo-, inotropic effects) ;
beta2-adrenergic receptors, which are located mainly in the bronchi, smooth muscle cells of the vascular wall, skeletal muscles, and in the pancreas; when they are stimulated, broncho- and vasodilatory effects, relaxation of smooth muscles and insulin secretion are realized;
beta3-adrenergic receptors, localized primarily on adipocyte membranes, are involved in thermogenesis and lipolysis.
The idea of using beta-blockers as cardioprotectors belongs to the Englishman J. W. Black, who in 1988, together with his collaborators, the creators of beta-blockers, was awarded the Nobel Prize. The Nobel Committee considered the clinical significance of these drugs to be “the greatest breakthrough in the fight against heart disease since the discovery of digitalis 200 years ago.”
Classification
Drugs from the group of beta-blockers differ in the presence or absence of cardioselectivity, intrinsic sympathetic activity, membrane-stabilizing, vasodilating properties, solubility in lipids and water, effect on platelet aggregation, and also in duration of action.
Currently, clinicians identify three generations of drugs with a beta-blocking effect.
I generation- non-selective beta1- and beta2-adrenergic blockers (propranolol, nadolol), which, along with negative ino-, chrono- and dromotropic effects, have the ability to increase the tone of the smooth muscles of the bronchi, vascular wall, and myometrium, which significantly limits their use in clinical practice.
II generation- cardioselective beta1-adrenergic blockers (metoprolol, bisoprolol), due to their high selectivity for beta1-adrenergic receptors of the myocardium, have more favorable tolerability with long-term use and a convincing evidence base for long-term prognosis of life in the treatment of hypertension, ischemic heart disease and heart failure.
Drugs III generation- celiprolol, bucindolol, carvedilol have additional vasodilating properties due to the blockade of alpha-adrenergic receptors, without intrinsic sympathomimetic activity.
Table. Classification of beta-blockers.
|
1. β 1 ,β 2 -AB (non-cardioselective) |
·anaprilin (propranolol) |
||
|
2. β 1 -AB (cardioselective) |
bisoprolol metoprolol |
||
|
3. AB with vasodilating properties |
β 1 ,α 1 -AB |
labetalol carvediol |
|
|
β 1 -AB (activation of NO production) |
nebivolol |
||
|
combination of blockade α 2 -adrenergic receptors and stimulation β 2 -adrenergic receptors |
celiprolol |
||
|
4. AB with internal sympathomimetic activity |
non-selective (β 1,β 2) |
pindalol |
|
|
selective (β 1) |
acebutalol talinolol epanolol |
||
Effects
The ability to block the effect of mediators on beta1-adrenergic receptors of the myocardium and the weakening of the effect of catecholamines on membrane adenylate cyclase of cardiomyocytes with a decrease in the formation of cyclic adenosine monophosphate (cAMP) determine the main cardiotherapeutic effects of beta-blockers.
Anti-ischemic effect of beta blockers is explained by a decrease in myocardial oxygen demand due to a decrease in heart rate (HR) and the force of heart contractions that occur when myocardial beta-adrenergic receptors are blocked.
Beta blockers simultaneously improve myocardial perfusion by reducing left ventricular (LV) end-diastolic pressure and increasing the pressure gradient that determines coronary perfusion during diastole, the duration of which increases as a result of a slower cardiac rhythm.
Antiarrhythmic action of beta blockers, based on their ability to reduce the adrenergic effect on the heart, leads to:
decrease in heart rate (negative chronotropic effect);
decreased automaticity of the sinus node, AV connection and the His-Purkinje system (negative bathmotropic effect);
reducing the duration of the action potential and the refractory period in the His–Purkinje system (the QT interval is shortened);
slowing down conduction in the AV junction and increasing the duration of the effective refractory period of the AV junction, lengthening the PQ interval (negative dromotropic effect).
Beta-blockers increase the threshold for the occurrence of ventricular fibrillation in patients with acute MI and can be considered as a means of preventing fatal arrhythmias in the acute period of MI.
Hypotensive action beta blockers are due to:
a decrease in the frequency and strength of heart contractions (negative chrono- and inotropic effects), which overall leads to a decrease in cardiac output (MCO);
decreased secretion and decreased concentration of renin in plasma;
restructuring of the baroreceptor mechanisms of the aortic arch and carotid sinus;
central depression of sympathetic tone;
blockade of postsynaptic peripheral beta-adrenergic receptors in the venous vascular bed, with a decrease in blood flow to the right side of the heart and a decrease in MOS;
competitive antagonism with catecholamines for receptor binding;
increased levels of prostaglandins in the blood.
The effect on beta2-adrenergic receptors determines a significant part of the side effects and contraindications to their use (bronchospasm, constriction of peripheral vessels). A feature of cardioselective beta-blockers compared to non-selective ones is their greater affinity for beta1-receptors of the heart than for beta2-adrenergic receptors. Therefore, when used in small and medium doses, these drugs have a less pronounced effect on the smooth muscles of the bronchi and peripheral arteries. It should be taken into account that the degree of cardioselectivity varies among different drugs. The index ci/beta1 to ci/beta2, characterizing the degree of cardioselectivity, is 1.8:1 for non-selective propranolol, 1:35 for atenolol and betaxolol, 1:20 for metoprolol, 1:75 for bisoprolol. However, it should be remembered that selectivity is dose-dependent; it decreases with increasing dosage of the drug.
In accordance with the clinically significant pharmacokinetic properties of beta-blockers, drugs are divided into 3 groups (see Table)
Table. Features of the metabolism of beta blockers.
* lipophilicity increases penetration through the blood-brain barrier; when central beta-1 receptors are blocked, vagal tone increases, which is important in the mechanism of antifibrillatory action. There is evidence (Kendall M.J. et al., 1995) that the reduction in the risk of sudden death is more pronounced when using lipophilic beta-blockers.
Indications:
IHD (MI, snocardia)
Tachyarrhythmias
Dissecting aneurysm
Bleeding from varicose veins of the esophagus (prevention for liver cirrhosis - propranolol)
Glaucoma (timolol)
Hyperthyroidism (propranolol)
Migraine (propranolol)
Alcohol withdrawal (propranolol)
Rules for prescribing β-AB:
start therapy with low doses;
increase the dose no more often than at 2-week intervals;
carry out treatment at the maximum tolerated dose;
1–2 weeks after the start of treatment and 1–2 weeks after completion of dose titration, monitoring of biochemical blood parameters is necessary.
If a number of symptoms appear while taking beta-blockers, follow the following recommendations:
if the symptoms of heart failure increase, the dose of the β-blocker should be halved;
in the presence of fatigue and/or bradycardia, reduce the dose of the β-blocker;
if a serious deterioration in health occurs, reduce the dose of the β-blocker by half or stop treatment;
at heart rate< 50 уд./мин следует снизить дозу β-адреноблокатора вдвое; при значительном снижении ЧСС лечение прекратить;
if the heart rate decreases, it is necessary to review the doses of other drugs that help slow the heart rate;
in the presence of bradycardia, it is necessary to promptly monitor ECG for early detection of heart block.
Side effects All β-blockers are divided into cardiac (bradycardia, arterial hypotension, development of atrioventricular block) and extracardiac (dizziness, depression, nightmares, insomnia, memory impairment, fatigue, hyperglycemia, hyperlipidemia, muscle weakness, impaired potency).
Stimulation of β2-adrenergic receptors leads to increased glycogenolysis in the liver and skeletal muscles, gluconeogenesis and insulin release. Therefore, the use of non-selective β-blockers may be accompanied by an increase in glycemia and the occurrence of insulin resistance. At the same time, in cases of type 1 diabetes mellitus, non-selective β-blockers increase the risk of “hidden hypoglycemia”, since after insulin administration they inhibit the return of glycemic levels to normal. Even more dangerous is the ability of these drugs to cause a paradoxical hypertensive reaction, which may be accompanied by reflex bradycardia. Such changes in hemodynamic status are associated with a significant increase in adrenaline levels due to hypoglycemia.
Another problem that may arise in the case of long-term use of non-selective β-blockers is a violation of lipid metabolism, in particular an increase in the concentration of very low-density lipoproteins, triglycerides and a decrease in the content of anti-atherogenic high-density lipoprotein cholesterol. These changes likely result from a weakening of the effects of lipoprotein lipase, which is normally responsible for the metabolism of endogenous triglycerides. Stimulation of unblocked α-adrenergic receptors against the background of blockade of β1 and β2-adrenergic receptors leads to inhibition of lipoprotein lipase, while the use of selective β-blockers makes it possible to prevent these lipid metabolism disorders. It should be noted that the beneficial effect of β-AB as cardioprotective agents (for example, after acute myocardial infarction) is much stronger and more important than the consequences of the adverse effects of these drugs on lipid metabolism.
Contraindications
Absolute contraindications for β-blockers are bradycardia (< 50–55 уд./мин), синдром слабости синусового узла, АВ-блокада II–III степени, гипотензия, острая сосудистая недостаточность, шок, тяжелая бронхиальная астма. Хронические обструктивные заболевания легких в стадии ремиссии, компенсированные заболевания периферических артерий в начальных стадиях, депрессия, гиперлипидемия, АГ у спортсменов и сексуально активных юношей могут быть относительными противопоказаниями для применения β-АБ. Если существует необходимость их назначения по показаниям, предпочтительно назначать малые дозы высокоселективных β-АБ.
Antagonistscalcium(AK) - a large group of drugs with different chemical structures, the common property of which is the ability to reduce the flow of ions calcium into vascular smooth muscle cells and cardiomyocytes, by interacting with slow calcium channels (L-type) of cell membranes. As a result, the smooth muscles of the arterioles relax, blood pressure and total peripheral vascular resistance decrease, the strength and frequency of heart contractions decrease, and atrioventricular (AV) conduction slows down.
AK classification:
|
Generation |
Dihydropyridine derivatives (atreria>heart) |
Phenylalkylamine derivatives (atreria<сердце) |
Benzothiazepine derivatives (atreria=heart) |
|
|
I generation (short-acting drugs) |
Nifedipine (Farmadipin, Corinfar) |
Verapamil(Isoptin, Lekoptin, Finoptin) |
Diltiazem |
|
|
II generation(retard forms) |
lek. forms) |
NifedipineS.R. NicardipineS.R. FelodipinS.R. |
VerapamilS.R. |
Diltiazem SR |
|
IIb active substances) |
Isradipin Nisoldipine Nimodipine Nivaldipin Nitrendipine | |||
|
IIIgeneration(only in the group of dihydropyridine derivatives) |
Amlodipine(Norvasc, Emlodin, Duactin, Normodipin, Amlo, Stamlo, Amlovas, Amlovask, Amlodak, Amlong, Amlopin, Tenox, etc.); Levorotatory amlodipine - Azomex Lacidipine(Lazipil), Lercanidipine(Lerkamen) Combined drugs: Equator, Gipril A (amlodipine + lisinopril) Tenochek(Amlodipine + atenolol) |
|||
Note: SR and ER are sustained release drugs
The main pharmacological effects of calcium antagonists:
Hypotensive effect (typical of derivatives of dihydropyridine, phenylalkylamine, benzothiazepine)
Antianginal (typical for derivatives of dihydropyridine, phenylalkylamine, benzothiazepine)
Antiarrhythmic effect (characteristic of the drugs verapamil and diltiazem).
Drugs belonging to different groups differ in the severity of their effect on the heart and peripheral vessels. Thus, dihydropyridine AKs act to a greater extent on blood vessels, and therefore they have a more pronounced hypotensive effect, and have virtually no effect on the conductivity of the heart and its contractile function. Verapamil has a high affinity for calcium channels of the heart, due to which it reduces the strength and frequency of heart contractions, worsens AV conduction, and has a lesser effect on blood vessels, so its hypotensive effect is less pronounced than that of dihydropyridine AKs. Diltiazem affects the heart and blood vessels equally. Since verapamil and diltiazem have a certain similarity with each other, they are conditionally grouped into a subgroup of non-dihydropyridine AAs. Within each group of AKs, short-acting drugs and prolonged drugs.
Currently, AKs are one of the main classes of drugs that can be used for the initial treatment of hypertension. According to comparative studies (ALLHAT, VALUE), prolonged AA demonstrated a hypotensive effect equal to the antihypertensive activity of ACE inhibitors, angiotensin II receptor antagonists, diuretics and β-blockers. The maximum reduction in blood pressure when taking AA is observed in low-renin, volume-dependent hypertension. AKs, in comparison with antihypertensive drugs of other classes (ACE inhibitors, diuretics and β-blockers), not only have an equal hypotensive effect, but also equally reduce the incidence of “major cardiovascular complications” - myocardial infarction, cerebral stroke and cardiovascular mortality. Left ventricular (LV) myocardial hypertrophy is an independent risk factor for hypertension. AKs reduce LV hypertrophy and improve its diastolic function, especially in patients with hypertension and coronary artery disease. An important aspect of the organoprotective effect of AA is the prevention or slowdown of vascular remodeling (the stiffness of the vascular wall decreases, endothelium-dependent vasodilation improves due to increased NO production).
A special approach is required in the treatment of hypertension in patients with diabetes mellitus (DM), since they have a particularly high risk of cardiovascular complications. When hypertension and diabetes are combined, the optimal antihypertensive drug should not only ensure the achievement of target blood pressure values, but also have pronounced organoprotective properties and be metabolically neutral. Long-acting dihydropyridine AA (felodipine, amlodipine, etc.), along with ACE inhibitors and ARBs, are the drugs of choice for the treatment of hypertension in patients with diabetes, since they not only effectively reduce blood pressure, but also have pronounced organoprotective properties, including nephroprotective effect (reduce the severity of microalbuminuria, slow down the progression of diabetic nephropathy), and are also metabolically neutral. In most patients with hypertension and diabetes, the target blood pressure level can be achieved only by using a combination of antihypertensive drugs. The most rational in this clinical situation are combinations of AK with ACE inhibitors or ARBs. It has now been convincingly shown (ASCOT-BPLA) that the use of drugs with favorable metabolic effects or metabolically neutral ones for the treatment of hypertension reduces the risk of developing diabetes by 30% compared with other antihypertensive drugs (thiazide diuretics, β-blockers). The results of these studies are reflected in the European clinical guidelines for the treatment of hypertension. Thus, when treating hypertension in patients with a high risk of developing diabetes (a family history of diabetes, obesity, impaired glucose tolerance), it is recommended to use drugs with a favorable metabolic profile (for example, long-acting AA, ACE inhibitors or ARB).
Indications:
Hypertension in pregnant women
Hypertension and supraventricular tachycardia*
Hypertension and migraine*
IHD (angina)
Hypertension in elderly patients
Systolic hypertension
Hypertension and peripheral artery disease
Hypertension and atherosclerosis of the carotid arteries
AH against the background of COPD and BR.Asthma
Contraindications:
AV block II-III degree*
* - only for non-dihydropyridine AKs
Relative contraindications:
* - only for non-dihydropyridine AKs
Effective combinations
Most multicenter studies have shown that in 70% of patients with hypertension, a combination of two or three antihypertensive drugs must be prescribed to achieve target blood pressure levels. Among combinations of two drugs, the following are considered effective and safe:
ACE inhibitor + diuretic,
BAB + diuretic,
AA + diuretic,
sartans + diuretic,
sartans + ACEI + diuretic
AK + ACEI,
Under hypertensive crisis understand all cases of sudden and significant increase in blood pressure, accompanied by the appearance or worsening of existing cerebral, cardiac or general vegetative symptoms, rapid progression of dysfunction of vital organs.
Criteria for hypertensive crisis:
relatively sudden onset;
individually high rise in blood pressure;
the appearance or intensification of complaints of a cardiac, cerebral or general vegetative nature.
In the USA and Europe, a clinical classification that is simple for choosing patient management tactics has become widespread, in which hypertensive crises are divided into complicated and uncomplicated.
Complicated hypertensive crises are characterized by acute or progressive target organ damage (TOD), pose a direct threat to the patient’s life and require an immediate, within 1 hour, reduction in blood pressure.
Uncomplicated hypertensive crises, there are no signs of acute or progressive POM, they pose a potential threat to the patient’s life, and require a rapid, within several hours, reduction in blood pressure.
Treatment of hypertensive crises
In the drug treatment of hypertensive crises, it is necessary to solve the following problems:
Relief of increased blood pressure. In this case, it is necessary to determine the degree of urgency of starting treatment, select the drug and method of its administration, set the required rate of blood pressure reduction, and determine the level of permissible blood pressure reduction.
Ensuring adequate monitoring of the patient's condition during the period of lowering blood pressure. Timely diagnosis of complications or excessive reduction in blood pressure is necessary.
Consolidation of the achieved effect. For this purpose, the same drug that was used to lower blood pressure is usually prescribed, and if this is not possible, other antihypertensive drugs are prescribed. The time is determined by the mechanism and duration of action of the selected drugs.
Treatment of complications and concomitant diseases.
Selection of the optimal dosage of medications for maintenance treatment.
Carrying out preventive measures to prevent crises.
Antihypertensive drugs.
Antihypotensive drugs are a group of drugs used to restore low blood pressure to normal. An acute drop in blood pressure (collapse, shock) can be a consequence of blood loss, injury, poisoning, infectious diseases, heart failure, dehydration, etc. In addition, chronic arterial hypotension can occur as an independent disease. To eliminate arterial hypotension, the following drugs are used:
increasing the volume of circulating blood - plasma expanders, saline solutions;
vasoconstrictors (caffeine, cordiamine, alpha-adrenergic agonists, glucocorticoids, mineralcorticoids, angiotensinamide);
improving tissue microcirculation and eliminating hypoxia - ganglion blockers, α-blockers;
non-glycoside cardiotonics (dobutamine, dopamine);
agents that have a tonic effect on the central nervous system - tinctures of lemongrass, ginseng, zamanikha, aralia; extracts of Eleutherococcus and Rhodiola rosea.
Drugs used for uncomplicated hypertensive crises
|
Drugs |
Doses and method Introductions |
actions |
Side effects |
|
Captopril |
12.5-25 mg orally or sublingually |
After 30 min. |
Orthostatic hypotension. |
|
Clonidine |
0.075-0.15 mg orally or 0.01% solution 0.5-2 ml IM or IV |
After 10-60 min. |
Dry mouth, drowsiness. Contraindicated in patients with AV block or bradycardia. |
|
Propranolol |
20 - 80 mg orally |
After 30-60 minutes. |
Bradycardia, bronchoconstriction. |
|
1% - 4-5 ml IV 0.5% - 8-10 ml IV |
After 10-30 minutes. |
More effective in combination with other antihypertensive drugs. |
|
|
Nifedipine |
5-10 mg orally or sublingually |
After 10-30 minutes. |
Headache, tachycardia, redness, possible development of angina. |
|
Droperidol |
0.25% solution 1 ml IM or IV |
After 10-20 minutes. |
Extrapyramidal disorders. |
Parenteral therapy for complicated hypertensive crises
|
Drug name |
Method of administration, dose |
Start of action |
Duration of action |
Note |
|
Clonidine |
IV 0.5-1.0 ml 0.01% solution or IM 0.5-2.0 ml 0.01% |
After 5-15 minutes. |
Undesirable for cerebral stroke. Bradycardia may develop. |
|
|
Nitroglycerine |
IV drip 50-200 mcg/min. |
After 2-5 minutes. |
Especially indicated for acute heart failure, MI. |
|
|
Enalapril |
IV 1.25-5 mg |
After 15-30 minutes. |
Effective in acute LV failure. |
|
|
Nimodipine |
After 10-20 minutes. |
For subarachnoid hemorrhages. |
||
|
Furosemide |
IV bolus 40-200 mg |
After 5-30 min. |
Mainly in hypertensive crises with acute cardiac or renal failure. |
|
|
Propranolol |
0.1% solution 3-5 ml in 20 ml physiological solution |
After 5-20 minutes. |
Bradycardia, AV block, bronchospasm. |
|
|
Magnesium sulfate |
IV bolus 25% solution |
After 30-40 minutes. |
For convulsions, eclampsia. |
|
Name of the drug, its synonyms, storage conditions and procedure for dispensing from pharmacies |
Release form (composition), quantity of the drug in the package |
Method of administration, average therapeutic doses |
|
Clonidine (clonidine) (List B) |
Tablets of 0.000075 and 0.00015 N.50 |
1 tablet 2-4 times a day |
|
Ampoules 0.01% solution 1 ml N.10 |
Under the skin (into the muscle) 0.5-1.5 ml Into a vein slowly 0.5-1.5 ml with 10-20 ml of 0.9% sodium chloride solution up to 3-4 times a day (in a hospital setting) |
|
|
Moxonidine (Physiotens) (List B) |
Tablets 0.001 |
1 tablet 1 time per day |
|
Methyldopa (dopegyt) (List B) |
Tablets of 0.25 and 0.5 |
1 tablet 2-3 times a day |
|
Reserpine (raucedil) |
Tablets 0.00025 |
1 tablet 2-4 times a day after meals |
|
(List B) |
Ampoules 0.25% solution 1 ml N.10 |
Into the muscle (into the vein slowly) 1 ml |
|
Prazosin (minipress) (List B) |
Tablets 0.001 and 0.005 N.50 |
½-5 tablets 2-3 times a day |
|
Atenolol (tenormin) (List B) |
Tablets 0.025; 0.05 and 0.1 N.50, 100 |
½-1 tablet 1 time per day |
|
Bisoprolol (List B) |
Tablets of 0.005 and 0.001 |
1 tablet 1 time per day |
|
Nifedipine (phenigidine, Corinfar) (List B) |
Tablets (capsules, dragees) 0.01 and 0.02 |
1-2 tablets (capsules, dragees) 3 times a day |
|
Sodium nitroprusside Sodium nitroprussidum (List B) |
Ampoules of 0.05 dry matter N.5 |
500 ml of 5% glucose solution drip into a vein |
|
Captopril (capoten) (List B) |
Tablets of 0.025 and 0.05 |
½-1 tablet 2-4 times a day before meals |
|
Magnesium sulfate Magnesii sulfas |
Ampoules 25% solution 5-10 ml N.10 |
Into the muscle (into the vein slowly) 5-20 ml |
|
"Adelfan" (List B) |
Official tablets |
½-1 tablet 1-3 times a day (after meals) |
|
"Brinerdin" (List B) |
Official dragees |
1 tablet 1 time per day (in the morning) |
A.Ya.Ivleva
Polyclinic No. 1 of the Medical Center of the Administration of the President of the Russian Federation, Moscow
Beta-blockers were first introduced into clinical practice 40 years ago as antiarrhythmic drugs and for the treatment of angina pectoris. Currently, they are the most effective means for secondary prevention after acute myocardial infarction (AMI). Their effectiveness has been proven as a means for the primary prevention of cardiovascular complications in the treatment of hypertension. In 1988, the creators of beta-blockers were awarded the Nobel Prize. The Nobel Committee assessed the importance of drugs of this group for cardiology as comparable to digitalis. Interest in the clinical study of beta-blockers turned out to be justified. Beta-adrenergic receptor blockade has become a therapeutic strategy for AMI, aimed at reducing mortality and reducing the infarct area. Over the past decade, it has been found that beta-blockers reduce mortality in chronic heart failure (CHF) and prevent cardiac complications during non-cardiac surgery. Controlled clinical studies have confirmed the high effectiveness of beta-blockers in special groups of patients, in particular those with diabetes mellitus and the elderly.
However, recent large-scale epidemiological studies (IMPROVEMENT, EUROASPIRE II and Euro Heart Failure survey) have shown that beta-blockers are used less frequently than they should in situations where they could be beneficial, so efforts are required to introduce modern preventive medicine strategies into medical practice from leading clinicians and scientists to explain the pharmacodynamic advantages of individual representatives of the group of beta-blockers and to substantiate new approaches to solving complex clinical problems, taking into account differences in the pharmacological properties of drugs.
Beta-blockers are competitive inhibitors of the binding of the transmitter of the sympathetic nervous system to beta-adrenergic receptors. Norepinephrine plays a critical role in the genesis of hypertension, insulin resistance, diabetes mellitus and atherosclerosis. The level of norepinephrine in the blood increases with stable and unstable angina, AMI and during the period of cardiac remodeling. In CHF, the level of norepinephrine varies over a wide range and increases as the NYHA functional class increases. With a pathological increase in sympathetic activity, a chain of progressive pathophysiological changes is initiated, the culmination of which is cardiovascular mortality. Increased sympathetic tone can provoke arrhythmias and sudden death. In the presence of a beta blocker, a higher concentration of norepinephrine agonist is required for the specific receptor to respond.
For the clinician, the most clinically accessible marker of increased sympathetic activity is a high resting heart rate (HR). In 20 large epidemiological studies involving more than 288,000 people, completed over the past 20 years, data have been obtained that a fast heart rate is an independent risk factor for cardiovascular mortality in the population as a whole and a prognostic marker for the development of coronary artery disease, hypertension, and diabetes mellitus . A generalized analysis of epidemiological observations made it possible to establish that in a cohort with a heart rate in the range of 90-99 beats/min, the mortality rate from complications of coronary heart disease and sudden death is 3 times higher compared to the population group with a heart rate less than 60 beats/min. It has been established that a high rhythm of cardiac activity is significantly more often recorded in arterial hypertension (AH) and ischemic heart disease. After an AMI, heart rate becomes an independent prognostic criterion for mortality both in the early post-infarction period and for mortality 6 months after AMI. Many experts consider the optimal heart rate to be up to 80 beats/min at rest, and the presence of tachycardia is stated when the heart rate is above 85 beats/min.
Studies of the level of norepinephrine in the blood, its metabolism and the tone of the sympathetic nervous system in normal and pathological conditions using high experimental technologies with the use of radioactive substances, microneurography, spectral analysis made it possible to establish that beta-blockers eliminate many of the toxic effects characteristic of catecholamines :
- oversaturation of the cytosol with calcium and protect myocytes from necrosis,
- stimulating effect on cell growth and apoptosis of cardiomyocytes,
- progression of myocardial fibrosis and left ventricular myocardial hypertrophy (LVMH),
- increased automatism of myocytes and fibrillatory action,
- hypokalemia and proarrhythmic effect,
- increased oxygen consumption by the myocardium in hypertension and LVMH,
- hyperreninemia,
- tachycardia.
There is a misconception that, with proper dosing, any beta blocker can be effective for angina, hypertension and arrhythmia. However, there are clinically important pharmacological differences between drugs in this group, such as selectivity for beta-adrenergic receptors, differences in lipophilicity, the presence of partial beta-agonist properties of beta-adrenergic receptors, as well as differences in pharmacokinetic properties that determine the stability and duration of action in clinical settings . Pharmacological properties of beta-blockers, presented in table. 1 may have clinical significance both when choosing a drug at the initial stage of use, and when switching from one beta-blocker to another.
The strength of binding to a specific receptor, or the strength of the binding of the drug to the receptor, determines the concentration of the mediator norepinephrine, which is required to overcome the competitive connection at the receptor level. As a result, the therapeutic doses of bisoprolol and carvedilol are lower than those of atenolol, metoprolol and propranolol, which have a less strong connection with the beta-adrenoreceptor.
The selectivity of blockers to beta-adrenergic receptors reflects the ability of drugs to varying degrees to block the effect of adrenomimetics on specific beta-adrenergic receptors in different tissues. Selective Beta-adrenergic locators include bisoprolol, betaxolol, nebivolol, metoprolol, atenolol, as well as the currently rarely used talinolol, oxprenolol and acebutolol. When used in low doses, Beta-adrenergic blockers exhibit the effects of blocking adrenergic receptors, which belong to the “Pj” subgroup, therefore their effect is manifested in organs in the tissue structures of which Beta-adrenergic receptors are predominantly represented, in particular in the myocardium, and have little effect on beta 2 - adrenergic receptors in the bronchi and blood vessels. However, at higher doses they also block beta-adrenergic receptors. In some patients, even selective beta-blockers can provoke bronchospasm, so the use of beta-blockers is not recommended for bronchial asthma. Correction of tachycardia in patients with bronchial asthma receiving beta-adrenergic agonists is clinically one of the most pressing and at the same time difficult to solve problems, especially with concomitant coronary heart disease (CHD), therefore, increasing the selectivity of beta-blockers is a particularly important clinical property for this group of patients . There is evidence that metoprolol succinate CR/XL has higher selectivity for beta-adrenergic receptors than atenolol. In a clinical experimental study, it had a significantly less effect on the forced expiratory volume in patients with bronchial asthma, and when using formaterol, it provided a more complete restoration of bronchial patency than atenolol.
Table 1.
Clinically important pharmacological properties of beta-blockers
|
A drug |
Strength of binding to the beta-adrenergic receptor (propranolol = 1.0) |
Relative beta receptor selectivity |
Intrinsic sympathomimetic activity |
Membrane-stabilizing activity |
|
Atenolol |
||||
|
Betaxolol |
||||
|
Bisoprolol |
||||
|
Bucindolol |
||||
|
Carvedilol* |
||||
|
Labetolol** |
||||
|
Metoprolol |
||||
|
Nebivolol |
No data |
|||
|
Penbutolol |
||||
|
Pindolol |
||||
|
Propranolol |
||||
|
Sotalol**** |
||||
Note. Relative selectivity (after Wellstern et al., 1987, cited in); * - carvedilol additionally has the property of a beta-blocker; ** - labetolol additionally has the property of an α-adrenergic blocker and the intrinsic property of a beta-adrenergic receptor agonist; *** - sotalol has additional antiarrhythmic properties
Selectivity for Beta-adrenergic receptors has important clinical significance not only for broncho-obstructive diseases, but also when used in patients with hypertension, with peripheral vascular diseases, in particular with Raynaud's disease and intermittent claudication. When using selective Beta-blockers, beta 2-adrenergic receptors, while remaining active, respond to endogenous catecholamines and exogenous adrenergic mimetics, which is accompanied by vasodilation. In special clinical studies, it was found that highly selective Beta-blockers do not increase the resistance of the vessels of the forearm, the femoral artery system, as well as the vessels of the carotid region and do not affect the tolerability of the step test for intermittent claudication.
Metabolic effects of beta blockers
With long-term (from 6 months to 2 years) use of non-selective beta-blockers, triglycerides in the blood increase in a wide range (from 5 to 2 5%) and cholesterol in the high-density lipoprotein fraction (HDL-C) decreases by an average of 13%. The effect of non-selective beta-adrenergic blockers on the lipid profile is associated with inhibition of lipoprotein lipase, since beta-adrenoreceptors, which reduce the activity of lipoprotein lipase, are without counter-regulation by beta 2-adrenoceptors, which are their antagonists in relation to this enzymatic system. At the same time, there is a slowdown in the catabolism of very low density lipoproteins (VLDL) and triglycerides. The amount of HDL cholesterol decreases because this fraction of cholesterol is a product of VLDL catabolism. Convincing information about the clinical significance of the effect of non-selective beta-adrenergic locators on the lipid profile has not yet been obtained, despite the huge number of observations of varying duration presented in the specialized literature. An increase in triglycerides and a decrease in HDL cholesterol are not typical for highly selective Beta-blockers; moreover, there is evidence that metoprolol slows down the process of atherogenesis.
Effect on carbohydrate metabolism mediated through beta 2 adrenergic receptors, since the secretion of insulin and glucagon, glycogenolysis in muscles and glucose synthesis in the liver are regulated through these receptors. The use of non-selective beta-blockers for type 2 diabetes mellitus is accompanied by an increase in hyperglycemia, and when switching to selective beta-blockers, this reaction is completely eliminated. Unlike non-selective beta-blockers, selective beta-blockers do not prolong insulin-induced hypoglycemia, since glycogenolysis and glucagon secretion are mediated through beta 2 -adrenergic receptors. In a clinical study, it was found that metoprolol and bisoprolol do not differ from placebo in their effect on carbohydrate metabolism in type 2 diabetes mellitus and no adjustment of hypoglycemic agents is required. However, insulin sensitivity is reduced when using all beta-blockers, and more significantly under the influence of non-selective beta-blockers.
Membrane stabilizing activity of beta-blockers caused by blockade of sodium channels. It is characteristic only of some beta-blockers (in particular, it is present in propranolol and some others that currently have no clinical significance). When using therapeutic doses, the membrane-stabilizing effect of beta-blockers has no clinical significance. It manifests itself as rhythm disturbances during intoxication due to overdose.
Presence of partial beta-adrenergic receptor agonist properties deprives the drug of its ability to reduce heart rate during tachycardia. As evidence accumulated of a reduction in mortality in patients who had suffered an AMI when treated with beta-blockers, the correlation between their effectiveness and a decrease in tachycardia became increasingly reliable. It was found that drugs with partial beta-adrenergic receptor agonist properties (oxprenolol, practolol, pindolol) had little effect on heart rate and mortality, in contrast to metoprolol, timolol, propranolol and atenolol. Subsequently, in the process of studying the effectiveness of beta-blockers in CHF, it was found that bucindolol, which has the properties of a partial agonist, did not change heart rate and did not have a significant effect on mortality, unlike metoprolol, carvedilol and bisoprolol.
Vasodilating effect present only in some beta-blockers (carvedilol, nebivolol, labetolol) and may have important clinical significance. For labetalol, this pharmacodynamic effect determined the indications and limitations for its use. However, the clinical significance of the vasodilatory effect of other beta-blockers (in particular, carvedilol and nebivalol) has not yet been fully clinically assessed.
Table 2.
Pharmacokinetic parameters of the most commonly used beta-blockers
Lipophilicity and hydrophilicity of beta-blockers determines their pharmacokinetic characteristics and ability to influence vagal tone. Water-soluble beta-blockers (atenolol, sotalol and nodalol) are eliminated from the body primarily through the kidneys and are little metabolized in the liver. Moderately lipophilic (bisoprolol, betaxolol, timolol) have a mixed elimination pathway and are partially metabolized in the liver. Highly lipophilic propranolol is metabolized in the liver by more than 60%, metoprolol is metabolized by the liver by 95%. The pharmacokinetic characteristics of the most commonly used beta-blockers are presented in table. 2. Specific pharmacokinetic properties of drugs may be clinically important. Thus, for drugs with very rapid metabolism in the liver, only a small part of the drug absorbed in the intestine enters the systemic circulation, therefore, when taken orally, the doses of such drugs are much higher than those used parenterally intravenously. Fat-soluble beta-blockers, such as propranolol, metoprolol, timolol and carvedilol, have genetically determined variability in pharmacokinetics, which requires more careful selection of the therapeutic dose.
Lipophilicity increases the penetration of beta-blocker through the blood-brain barrier. It has been experimentally proven that blockade of central Beta-adrenergic receptors increases vagal tone, and this is important in the mechanism of antifibrillatory action. There is clinical evidence that the use of drugs that are lipophilic (clinically proven for propranolol, timolol and metoprolol) is accompanied by a more significant reduction in the incidence of sudden death in high-risk patients. The clinical significance of lipophilicity and the ability of the drug to penetrate the blood-brain barrier cannot be considered fully established in relation to such central effects as drowsiness, depression, hallucinations, since it has not been proven that water-soluble beta 1 adrenergic blockers, such as atenolol, cause fewer such undesirable effects .
It is clinically important that:
- in case of impaired liver function, in particular due to heart failure, as well as when used together with drugs that compete with lipophilic beta-blockers in the process of metabolic biotransformation in the liver, the dose or frequency of taking lipophilic fS-blockers should be reduced.
- in case of severe renal impairment, dose reduction or adjustment of the frequency of taking hydrophilic beta-blockers is required.
Stability of action of the drug, the absence of pronounced fluctuations in blood concentration is an important pharmacokinetic characteristic. Improvements in the dosage form of metoprolol have led to the creation of a drug with controlled slow release. Metoprolol succinate CR/XL provides a stable concentration in the blood for 24 hours without sudden increases in content. At the same time, the pharmacodynamic properties of metoprolol also change: metoprolol CR/XL has been clinically shown to increase selectivity to Beta-adrenergic receptors, since in the absence of peak fluctuations in concentration, less sensitive beta 2-adrenergic receptors remain completely intact.
Clinical value of beta blockers in AMI
The most common cause of death in AMI is rhythm disturbances. However, the risk remains elevated, and in the post-infarction period most deaths occur suddenly. For the first time, in the randomized clinical trial MIAMI (1985), it was found that the use of the beta-blocker metoprolol in AMI reduces mortality. Metoprolol was administered intravenously against the background of AMI, followed by oral administration of this drug. Thrombolysis was not performed. There was a 13% decrease in mortality over 2 weeks compared to the group of patients receiving placebo. Later, in the controlled trial TIMI P-V, intravenous metoprolol was used against the background of thrombolysis and achieved a reduction in recurrent infarctions in the first 6 days from 4.5 to 2.3%.
When using beta-blockers for AMI, the frequency of life-threatening ventricular arrhythmias and ventricular fibrillation is significantly reduced, and the syndrome of prolongation of the Q-T interval that precedes fibrillation develops less frequently. As shown by the results of randomized clinical trials - VNAT (propranolol), the Norwegian study (timolol) and the Gothenburg study (metoprolol) - the use of a beta-blocker can reduce the mortality rate from repeated AMI and the frequency of repeated non-fatal myocardial infarction (MI) in the first 2 weeks on average by 20-25%.
Based on clinical observations, recommendations have been developed for the intravenous use of beta-blockers in the acute period of MI in the first 24 hours. Metoprolol, the most studied clinically in AMI, is recommended to be used intravenously at a dose of 5 mg over 2 minutes with a break of 5 minutes, for a total of 3 doses. Then the drug is prescribed orally at 50 mg every 6 hours for 2 days, and subsequently at 100 mg 2 times a day. In the absence of contraindications (heart rate less than 50 beats/min, SAP less than 100 mm Hg, blockade, pulmonary edema, bronchospasm, or if the patient received verapamil before the development of AMI), treatment is continued for a long time.
It was found that the use of drugs that are lipophilic (proven for timolol, metoprolol and propranolol) is accompanied by a significant reduction in the incidence of sudden death in AMI in high-risk patients. In table Table 3 presents data from controlled clinical studies assessing the clinical effectiveness of lipophilic beta-blockers for coronary artery disease in reducing the incidence of sudden death in AMI and in the early post-infarction period.
Clinical value of beta-blockers as agents for secondary prevention in ischemic heart disease
In the post-infarction period, the use of beta-blockers provides a significant, on average 30%, reduction in cardiovascular mortality in general. According to the Gothenburg study and meta-analysis, the use of metoprolol reduces mortality in the post-infarction period by 36-48%, depending on the level of risk. beta-blockers are the only group of drugs for drug prevention of sudden death in patients who have suffered AMI. However, not all beta blockers are created equal.
Table 3.
Controlled clinical trials showing a reduction in sudden death with the use of lipophilic beta-blockers in AMI
In Fig. Table 1 presents generalized data on the reduction in mortality in the post-infarction period recorded in randomized clinical trials using beta-blockers with grouping depending on the presence of additional pharmacological properties.
A meta-analysis of data from placebo-controlled clinical trials showed a significant reduction in mortality by an average of 22% with long-term use of beta-blockers in patients who had previously suffered an AMI, the incidence of reinfarction by 27%, and a reduction in the incidence of sudden death, especially in the early morning hours, by an average of 30 %. Mortality after AMI in patients treated with metoprolol in the Gothenburg study who had symptoms of heart failure was reduced by 50% compared with the placebo group.
The clinical effectiveness of beta-blockers has been established both after transmural MI and in persons who have suffered AMI without Q on the ECG. The effectiveness is especially high in patients from a high-risk group: smokers, the elderly, with CHF, diabetes mellitus.
The differences in the antifibrillatory properties of beta-blockers are more convincing when comparing the results of clinical studies using lipophilic and hydrophilic drugs, in particular the results recorded with the use of water-soluble sotalol. Clinical data suggest that lipophilicity is an important property of the drug, which at least partly explains the clinical value of beta-blockers in the prevention of sudden arrhythmic death in AMI and in the post-infarction period, since their vagotropic antifibrillatory effect is of central origin.
With long-term use of lipophilic beta-blockers, a particularly important property is the weakening of stress-induced suppression of vagal tone and increased vagotropic effect on the heart. The preventive cardioprotective effect, in particular the reduction of sudden death in the long-term post-infarction period, is largely due to this effect of beta-blockers. In table Table 4 presents data on lipophilicity and cardioprotective properties established in controlled clinical studies in ischemic heart disease.
The effectiveness of beta-blockers in ischemic heart disease is explained by both their antifibrillatory, antiarrhythmic, and anti-ischemic actions. beta-blockers have a beneficial effect on many mechanisms of myocardial ischemia. It is also believed that beta-blockers can reduce the likelihood of rupture of atheromatous formations with subsequent thrombosis.
In clinical practice, the doctor should focus on changes in heart rate during therapy with beta-blockers, the clinical value of which is largely due to their ability to reduce heart rate during tachycardia. In current international expert recommendations for the treatment of coronary artery disease with the use of beta-blockers, the target heart rate is from 55 to 60 beats/min, and in accordance with the recommendations of the American Heart Association, in severe cases, the heart rate can be reduced to 50 beats/min or less.
The work of Hjalmarson et al. The results of a study of the prognostic value of heart rate in 1807 patients admitted with AMI are presented. The analysis included both patients with subsequently developing CHF and those without hemodynamic impairment. Mortality was assessed for the period from the second day of hospitalization to 1 year. It was found that a frequent heart rhythm has an unfavorable prognosis. At the same time, the following mortality rates were recorded during the year depending on the heart rate at admission:
- at heart rate 50-60 beats/min - 15%;
- with heart rate above 90 beats/min - 41%;
- with heart rate above 100 beats/min - 48%.
In the large-scale GISSI-2 study with 8915 patients over a 6-month follow-up period, 0.8% of deaths were reported in the group with a heart rate less than 60 beats/min during the thrombolysis period and 14% in the group with a heart rate above 100 beats/min. The results of the GISSI-2 study confirm observations from the 1980s. about the prognostic value of heart rate in AMI, which was treated without thrombolysis. The project coordinators proposed including heart rate as a prognostic criterion in the clinical characteristics and considering beta-blockers as first-choice drugs for preventive treatment of patients with coronary artery disease and high heart rate.
In Fig. Figure 2 shows the dependence of the incidence of recurrent myocardial infarction when using beta-blockers with different pharmacological properties for the secondary prevention of complications of coronary artery disease, according to randomized controlled trials.
Clinical value of beta-blockers in the treatment of hypertension
A number of large-scale randomized clinical trials (SHEP Cooperative Research Group, 1991; MRC Working Party, 1992; IPPPSH, 1987; HAPPHY, 1987; MAPHY, 1988; STOP Hypertension, 1991) found that the use of beta-blockers as antihypertensive drugs is accompanied by a decrease in the incidence of cardiovascular mortality in both young and older age groups. International expert recommendations classify beta-blockers as first-line drugs for the treatment of hypertension.
Ethnic differences in the effectiveness of beta-blockers as antihypertensive agents have been identified. In general, they are more effective in controlling blood pressure in young white patients and at high heart rates.
Rice. 1.
Reduction of mortality when using beta-blockers after myocardial infarction, depending on additional pharmacological properties.
Table 4.
Lipophilicity and cardioprotective effect of beta-blockers to reduce mortality during long-term use for the purpose of secondary prevention of cardiac complications in coronary artery disease
Rice. 2.
The relationship between a decrease in heart rate when using various beta-blockers and the incidence of reinfarction (according to randomized clinical trials: Pooling Project).
The results of the multicenter randomized comparative study MAPHY, which was devoted to the study of primary prevention of atherosclerotic complications in the treatment of hypertension with metoprolol and a thiazide diuretic in 3234 patients for an average of 4.2 years, proved the advantage of therapy with the selective beta-blocker metoprolol. Overall mortality and mortality from coronary complications was significantly lower in the group receiving metoprolol. Non-CVD mortality was similar in the metoprolol and diuretic groups. In addition, in the group of patients receiving lipophilic metoprolol as the main antihypertensive agent, the incidence of sudden death was significantly 30% lower than in the group receiving a diuretic.
In a similar comparative study, HAPPHY, most patients received the selective hydrophilic beta-blocker atenolol as an antihypertensive agent, and no significant benefit was established with beta-blockers or diuretics. However, in a separate analysis and in this study, in the subgroup receiving metoprolol, its effectiveness in preventing cardiovascular complications, both fatal and non-lethal, was significantly higher than in the group receiving diuretics.
In table Table 5 presents the effectiveness of beta-blockers that have been documented in controlled clinical trials when used for the primary prevention of cardiovascular complications in the treatment of hypertension.
Until now, there is no complete understanding of the mechanism of the antihypertensive action of beta-blockers. However, the observation that the average heart rate in the population of people with hypertension is higher than that of the normotensive population is practically important. A comparison of 129,588 normotensive and hypertensive individuals in the Framingham Study revealed that not only was the mean heart rate higher in the hypertensive group, but mortality during follow-up increased as heart rate increased. This pattern is observed not only in young patients (18-30 years old), but also in the middle age group up to 60 years old, as well as in patients over 60 years old. An increase in sympathetic tone and a decrease in parasympathetic tone is recorded on average in 30% of patients with hypertension and, as a rule, in association with metabolic syndrome, hyperlipidemia and hyperinsulinemia, and for such patients the use of beta-blockers can be considered pathogenetic therapy.
Hypertension itself is only a weak predictor of the risk of developing coronary artery disease for a particular patient, but the association with blood pressure, especially systolic blood pressure, is independent of the presence of other risk factors. The relationship between blood pressure level and the risk of coronary artery disease is linear. Moreover, in patients whose blood pressure decreases at night by less than 10% (non-dippers), the risk of coronary artery disease increases 3 times. Among the numerous risk factors for the development of IHD, hypertension acquires a major role due to its prevalence, as well as due to the common pathogenetic mechanisms of cardiovascular complications in hypertension and IHD. Many risk factors, such as dyslipidemia, insulin resistance, diabetes mellitus, obesity, sedentary lifestyle, and some genetic factors, are important in the development of both coronary artery disease and hypertension. In general, patients with hypertension have a higher number of risk factors for the development of coronary artery disease than those with normal blood pressure. Among the 15% of the general adult population with hypertension, ischemic heart disease is the most common cause of death and disability. An increase in sympathetic activity in hypertension contributes to the development of LVMH and the vascular wall, stabilization of high blood pressure levels and a decrease in coronary reserve with an increased tendency to coronary spasm. Among patients with coronary artery disease, the frequency of hypertension is 25% and an increase in pulse pressure is a highly aggressive risk factor for coronary death.
Reducing blood pressure in hypertension does not completely eliminate the increased risk of mortality from coronary artery disease in patients with hypertension. A meta-analysis based on the results of treatment for 5 years in 37,000 patients with moderate hypertension who did not suffer from coronary artery disease showed that with blood pressure correction, coronary mortality and non-fatal complications of coronary artery disease are reduced by only 14%. In a meta-analysis that included data on the treatment of hypertension in people over 60 years of age, a 19% reduction in the incidence of coronary events was found.
Treatment of hypertension in patients with coronary artery disease should be more aggressive and more individualized than in its absence. The only group of drugs that have a proven cardioprotective effect against coronary artery disease when used for secondary prevention of coronary complications are beta-blockers, regardless of the presence of concomitant hypertension in patients.
Prognostic criteria for the high effectiveness of beta-blockers in ischemic heart disease are high heart rate before drug use and low rhythm variability. As a rule, in such cases there is also low tolerance to physical activity. Despite the favorable changes in myocardial perfusion due to a decrease in tachycardia under the influence of beta-blockers in ischemic heart disease and hypertension, in severe patients with concomitant hypertension and LVMH, a decrease in myocardial contractility may be the most important element in the mechanism of their antianginal action.
Among antihypertensive drugs, the reduction of myocardial ischemia is a property inherent only to beta-blockers, therefore their clinical value in the treatment of hypertension is not limited to the ability to correct blood pressure, since many patients with hypertension are also patients with coronary artery disease or at high risk of developing it. The use of beta-blockers is the most reasonable choice of pharmacotherapy to reduce coronary risk in hypertension in patients with sympathetic hyperactivity.
The clinical value of metoprolol has been fully proven (level A) as a means for the primary prevention of cardiovascular complications in hypertension, its antiarrhythmic effect and a reduction in the incidence of sudden death in hypertension and coronary heart disease have been documented (Gothenburg study; Norwegian study; MAPHY; MRC; IPPPSH; VNAT) .
Drugs for the treatment of hypertension are currently required to have a stable hypotensive effect when taken once a day. The pharmacological properties of the lipophilic selective Beta-blocker metoprolol succinate (CR/XL) in a new dosage form with a daily hypotensive effect fully meet these requirements. The dosage form of metoprolol succinate (CR/XL) is a tablet developed on the basis of high pharmaceutical technology, containing several hundred capsules of metoprolol succinate. After entering the stomach, each
Table 5.
Cardioprotective effect of beta-blockers during long-term use for the prevention of cardiovascular complications in hypertension
The capsule, under the influence of gastric contents, disintegrates in the mode specified for it to penetrate the gastric mucosa and works as an independent system for delivering the drug into the bloodstream. The absorption process occurs within 20 hours and does not depend on the pH in the stomach, its motility and other factors.
Clinical value of beta-blockers as antiarrhythmic agents
Beta-blockers are the drugs of choice for the treatment of supraventricular and ventricular arrhythmias, as they do not have the proarrhythmic effect characteristic of most specific antiarrhythmic drugs.
Supraventricular arrhythmias in hyperkinetic conditions, such as sinus tachycardia during excitement, thyrotoxicosis, mitral valve stenosis, ectopic atrial tachycardia and paroxysmal supraventricular tachycardia, often provoked by emotional or physical stress, are eliminated by beta-blockers. In new-onset atrial fibrillation and flutter, beta blockers may restore sinus rhythm or slow heart rate without restoring sinus rhythm due to an increase in the AV node refractory period. beta-blockers effectively control heart rate in patients with a permanent form of atrial fibrillation. In the placebo-controlled METAFER trial, metoprolol CR/XL was shown to be effective in stabilizing rhythm after cardioversion in patients with atrial fibrillation. The effectiveness of beta-blockers is not inferior to the effectiveness of cardiac glycosides for atrial fibrillation; in addition, cardiac glycosides and beta-blockers can be used in combination. For rhythm disturbances resulting from the use of cardiac glycosides, beta-blockers are the drugs of choice.
Ventricular arrhythmias, such as ventricular extrasystoles, as well as paroxysms of ventricular tachycardia, developing with ischemic heart disease, physical activity, and emotional stress, are usually eliminated with beta-blockers. Of course, ventricular fibrillation requires cardioversion, but for recurrent ventricular fibrillation provoked by physical exertion or emotional stress, especially in children, beta-blockers are effective. Post-infarction ventricular arrhythmias can also be treated with beta-blockers. Ventricular arrhythmias due to mitral valve prolapse and long QT syndrome are effectively treated with propranolol.
Rhythm disturbances during surgical operations and in the postoperative period are usually transient in nature, but if they are long-lasting, the use of beta-blockers is effective. In addition, beta blockers are recommended for the prevention of such arrhythmias.
Clinical value of beta-blockers in CHF
New recommendations from the European Society of Cardiology for the diagnosis and treatment of CHF and the American Heart Association were published in 2001. The principles of rational treatment of heart failure are summarized by leading cardiologists in our country. They are based on evidence-based medicine and highlight for the first time the important role of beta-blockers in combination pharmacotherapy for the treatment of all patients with mild, moderate and severe heart failure with reduced ejection fraction. Long-term treatment with beta-blockers is also recommended for left ventricular systolic dysfunction after AMI, regardless of the presence or absence of clinical manifestations of CHF. The officially recommended drugs for the treatment of CHF are bisoprolol, metoprolol in slow-release dosage form CR/XL and carvedilol. All three beta-blockers (metoprolol CR/XL, bisoprolol and carvedilol) were found to reduce the risk of mortality in CHF, regardless of the cause of death, by an average of 32-34%.
In patients enrolled in the MERIT-HE study who received slow-release metoprolol, mortality from cardiovascular causes decreased by 38%, the incidence of sudden death decreased by 41%, and mortality from increasing CHF decreased by 49%. All this data was highly reliable. Tolerability of metoprolol in the slow-release dosage form was very good. Drug withdrawal occurred in 13.9%, and in the placebo group - in 15.3% of patients. Due to side effects, 9.8% of patients stopped taking metoprolol CR/XL, 11.7% stopped taking placebo. Discontinuation due to worsening CHF occurred in 3.2% of the group receiving extended-release metoprolol and 4.2% of those receiving placebo.
The effectiveness of metoprolol CR/XL for CHF was confirmed in patients younger than 69.4 years (average age in the subgroup was 59 years) and in patients older than 69.4 years (average age in the older subgroup was 74 years). The effectiveness of metoprolol CR/XL has also been demonstrated in CHF with concomitant diabetes mellitus.
In 2003, data from the CO-MET trial were published in 3029 patients with CHF comparing carvedilol (target dose 25 mg twice daily) with immediate-release and low-dose metoprolol tartrate (50 mg twice daily). not corresponding to the required therapy regimen to ensure sufficient and stable concentrations of the drug throughout the day. The study, as would be expected under such circumstances, showed the superiority of carvedilol. However, its results are not of clinical value, since the MERIT-HE study demonstrated the effectiveness of metoprolol succinate in a slow-release dosage form for a single daily dose of 159 mg/day in reducing mortality in CHF (with a target dose of 200 mg /day).
Conclusion
The purpose of this review is to emphasize the importance of a thorough physical examination of the patient and assessment of his condition when choosing pharmacotherapy tactics. To use beta-blockers, emphasis should be placed on identifying hypersympathicotonia, which often accompanies the most common cardiovascular diseases. Currently, there is insufficient data to validate heart rate as a primary target for pharmacological correction in ischemic heart disease, hypertension and heart failure. However, the hypothesis about the importance of reducing heart rate in the treatment of hypertension and coronary artery disease has already been scientifically substantiated. The use of beta-blockers allows you to balance the increased energy consumption during tachycardia, accompanying hypersympathicotonia, correct pathological remodeling of the cardiovascular system, delay or slow down the progression of functional failure of the myocardium due to dysfunction of the beta-adrenergic receptors themselves (down-regulation) and a decrease in the response to catecholamines with a progressive decrease contractile function of cardiomyocytes. In recent years, it has also been established that an independent prognostic risk factor, especially in patients who have suffered an AMI with indicators of reduced left ventricular contractility, is reduced heart rate variability. It is believed that the initiating factor in the development of ventricular tachycardia in this category of patients is an imbalance of sympathetic and parasympathetic regulation of the heart. The use of the beta-blocker metoprolol in patients with coronary artery disease leads to an increase in rhythm variability mainly due to an increase in the influence of the parasympathetic nervous system.
The reasons for excessive caution in prescribing beta-blockers are often concomitant diseases (in particular, left ventricular dysfunction, diabetes mellitus, old age). However, it was found that the maximum effectiveness of the selective Beta-blocker metoprolol CR/XL was registered precisely in these groups of patients.
Literature
1. EUROASP1REII Study Group Lifestyle and risk factor management and use of dnig therapies in coronary patients from 15 countries. Eur Heart J 2001; 22: 554-72.
2. Mapee BJO. Journal heart missing items 2002; 4 (1): 28-30.
3. Task Force of the European Society of Cardiology and the North American Sod - ety of Pacing and Electrophysiology. Circulation 1996; 93: 1043-65. 4. Kannel W, Kannel C, Paffenbarger R, Cupples A. Am Heart J 1987; 113: 1489-94.
5. Singh BN.J Cardiovascular Pharmacol Therapeutics 2 001; 6 (4): 313 -31.
6. Habib GB. Cardiovascular Med 2001; 6:25-31.
7. CndckshankJM, Prichard BNC. Beta-blockers in clinical practice. 2nd edition. Edinburgh: Churchill-Livingstone. 1994;p. 1-1204.
8. Lofdahl C-G, Daholf C, Westergren G et aL EurJ Clin Pharmacol 1988; 33 (SllppL): S25-32.
9. Kaplan JR, Manusk SB, Adams MR, Clarkson TV. Eur Heart J 1987; 8: 928-44.
1 O.Jonas M, Reicher-Reiss H, Boyko Vetal.Fv) Cardiol 1996; 77: 12 73-7.
U. Kjekshus J. Am J Cardiol 1986; 57:43F-49F.
12. ReiterMJ, ReiffelJAAmJ Cardiol 1998; 82(4A):91-9-
13- Head A, Kendall MJ, Maxwell S. Clin Cardiol 1995; 18: 335-40.
14- Lucker P.J Clin Pharmacol 1990; 30 (siippl.): 17-24-
15- The MIAMI Trial Research Group. 1985. Metoprolol in acute myocardial infarction (MIAMI). A randomized placebo controlled international trial. Eur Heart J 1985; 6: 199-226.
16. RobertsR, Rogers WJ, MuellerHS et al. Circulation 1991; 83: 422-37.
17. Norwegian Study Group. Timolol-induced reduction in mortality and rein-farction in patients surviving acute myocardial infarction. NEngl J Med 1981; 304:801-7.
18. Beta-blockers Heart Attack Trial Research Group. A randomized trial of pro-pranolol in patients with acute myocardial infarction: mortality resuUs. JAMA 1982; 247:1707-13. 19- Olsson G, Wikstrand J, Warnoldl et al. Eur HeartJ 1992; 13:28-32.
20. Kennedy HL, Brooks MM, Barker AH etalAmJ Cardiol 1997; 80:29J-34J.
21. Kendall MJ, Lynch KP, HjalmarsonA, Kjekshus J.Ann Intern Med 1995; 123: 358-67.
22. Frishman WH. Postinfarction survival: Role of beta-adrenergic blockade, in Fuster V (ed): Atherosclerosis and Coronary Artery Disease. Philadelphia, Lip-pencott, 1996; 1205-14-
23. YusufS, WittesJ, Friedman L.J Am Med Ass 1988; 260:2088-93. 24.Julian DG, Prescott RJJackson FS. Lancet 1982; i: 1142-7.
25. KjekshusJ. Am J Cardiol 1986; 57: 43F-49F.
26. Soriano JB, Hoes AW, Meems L Prog Cardiovasc Dis 199 7; XXXIX: 445-56. 27.AbladB, Bniro T, BjorkmanJA etalJAm Coll Cardiol 1991; 17 (Suppl): 165.
28. HjalmarsonA, ElmfeldtD, HerlitzJ et al. Lancet 1981; ii: 823-7.
29. HjalmarsonA, Gupin E, Kjekshus J etal. AmJ Cardiol 1990; 65: 547-53.
30. Zuanetti G, Mantini L, Hemandesz-Bemal F et al. Eur Heart J 1998; 19 (Suppl): F19-F26.
31. Beta-Blocker Pooling Project Research Group (BBPP). Subgroup findings from randomized trials in post infarction patients. Eur Heart J 1989; 9: 8-16. 32.2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension.) Hypertension 2003; 21: 1011-53.
33.HolmeI, Olsson G, TuomilehtoJ et alJAMA 1989; 262:3272-3.
34. Wtthelmsen L, BerghmdG, ElmfeldtDetalJHypertension 1907; 5: 561-72.
35- The IPPPSH Collaborative Group. Cardiovascular risk and risk factors in a randomized trial of treatment based on the beta blocker oxprenololj Hyperten - sion 1985; 3:379-92.
36. Medical Research Council Working Party trial of treatment of hypertension in older adults: principal results. BMJ 1992; 304:405-12.
37- Velenkov YN., Mapeee VYu. Principles of rational treatment of heart failure M: Media Medica. 2000; pp. 149-55-
38. Wikstrand J, Warnoldl, Olsson G et al. JAMA 1988; 259: 1976-82.
39. Gillman M, Kannel W, Belanger A, D"Agostino R. Am Heart J1993; 125: 1148-54.
40. Julius S. Eur HeartJ 1998; 19 (suppLF): F14-F18. 41. Kaplan NMJ Hypertension 1995; 13 (suppl.2): S1-S5. 42.McInnesGT.JHypertens 1995; 13 (suppl.2):S49-S56.
43. Kannel WB J Am Med Ass 1996;275:1571-6.
44. Franklin SS, Khan SA, Wong ND, Larson MG. Circulation 1999; 100: 354-460.
45. Verdecchia P, Porcellatti C, Schilatti C et al. Hypertension 1994; 24:967-78.
46. Collins R, McMahon S. Br Med Bull 1994; 50:272 -98.
47. Collins R, Peto R, McMahon S et al. Lancet 1990; 335: 82 7-38.
48. McMahon S, Rodgers A Clin Exp Hypertens 1993; 15: 967-78.
49. First international study of infarct survival collaborative group. Lancet 1986; 2: 57-66.
50. The beta-blocker pooling project research group. Eur Heart J 1988; 9: 8-16.
51. Patatini P, Casiglia E, Julius S, Pesina AC. Arch Int Med 1999; 159: 585 -92.
52. Kueblkamp V, Schirdewan A, Stangl K et al. Circulation 1998; 98 Suppl. I: 1-663.
53.Remme WJ, Swedberg K. Eur HeartJ 2001; 22: 1527-260.
54. HuntSA.ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult: Executive Summary. Circulation 2001; 104:2996-3007.
55.Andersson B, Aberg J.J Am Coy Cardiol 1999; 33: 183A-184A.
56. BouzamondoA, HulotJS, Sanchez P et al. Eur J Heart failure 2003; 5: 281-9.
57. Keeley EC, Page RL, Lange RA et al. AmJ Cardiol 1996; 77: 557-60.
Medicines Index
Metoprolol succinate: BETALOK ZOK (AstraZeneca)
Beta-adrenergic receptor blockers, commonly known as beta blockers, are an important group of hypertension medications that act on the sympathetic nervous system. These drugs have been used in medicine for a long time, since the 1960s. The discovery of beta blockers has significantly increased the effectiveness of treating cardiovascular diseases, as well as hypertension. Therefore, the scientists who were the first to synthesize and test these drugs in clinical practice were awarded the Nobel Prize in Medicine in 1988.

In the practice of treating hypertension, beta blockers are still medications of primary importance, along with diuretics, i.e. diuretics. Although, since the 1990s, new groups of drugs have also appeared (calcium antagonists, ACE inhibitors), which are prescribed when beta blockers do not help or are contraindicated for the patient.

Popular medicines:
History of discovery
In the 1930s, scientists discovered that it was possible to stimulate the ability of the heart muscle (myocardium) to contract if it was exposed to special substances - beta-agonists. In 1948, the concept of the existence of alpha and beta adrenergic receptors in the mammalian body was put forward by R. P. Ahlquist. Later, in the mid-1950s, scientist J. Black theoretically developed a way to reduce the frequency of angina attacks. He suggested that it would be possible to invent a drug that would effectively “protect” the beta receptors of the heart muscle from the influence of adrenaline. After all, this hormone stimulates the muscle cells of the heart, causing them to contract too intensely and causing heart attacks.
In 1962, under the leadership of J. Black, the first beta blocker, protenalol, was synthesized. But it turned out to cause cancer in mice, so it was not tested on humans. The first medicine for humans was propranolol, which appeared in 1964. For the development of propranolol and the “theory” of beta blockers, J. Black received the Nobel Prize in Medicine in 1988. The most modern drug in this group, nebivolol, was launched on the market in 2001. It and other third-generation beta blockers have the additional important benefit of relaxing blood vessels. In total, more than 100 different beta blockers were synthesized in laboratories, but no more than 30 of them were or are still used by practicing physicians.

Mechanism of action of beta blockers
The hormone adrenaline and other catecholamines stimulate beta-1 and beta-2 adrenergic receptors, which are found in various organs. The mechanism of action of beta blockers is that they block beta-1 adrenergic receptors, “shielding” the heart from the effects of adrenaline and other “accelerating” hormones. As a result, the work of the heart becomes easier: it contracts less frequently and with less force. Thus, the frequency of angina attacks and heart rhythm disturbances is reduced. The likelihood of sudden cardiac death is reduced.
Beta blockers lower blood pressure through several different mechanisms simultaneously:
- Decreased heart rate and strength;
- Decreased cardiac output;
- Decreased secretion and decreased concentration of renin in the blood plasma;
- Restructuring of the baroreceptor mechanisms of the aortic arch and sinocarotid sinus;
- Depressant effect on the central nervous system;
- Effect on the vasomotor center - decreased central sympathetic tone;
- Decreased peripheral vascular tone due to alpha-1 receptor blockade or nitric oxide (NO) release.
Beta-1 and beta-2 adrenergic receptors in the human body
| Adrenergic receptor type | Localization | Stimulation result |
|---|---|---|
| Beta 1 receptors | Sinus node | Increased excitability, increased heart rate |
| Myocardium | Increased contraction strength | |
| Coronary arteries | Extension | |
| Atrioventricular node | Increased conductivity | |
| Bundle and pedicles of His | Increased automation | |
| Liver, skeletal muscles | Increased glycogenesis | |
| Beta 2 receptors | Arterioles, arteries, veins | Relaxation |
| Bronchial muscles | Relaxation | |
| Pregnant woman's uterus | Weakening and stopping contractions | |
| Islets of Langerhans (pancreatic beta cells) | Increased insulin secretion | |
| Adipose tissue (also contains beta-3 adrenergic receptors) | Increased lipolysis (the breakdown of fats into their constituent fatty acids) | |
| Beta 1 and beta 2 receptors | Juxtaglomerular apparatus of the kidneys | Increased renin release |
From the table we see that beta-1 adrenergic receptors are found, for the most part, in the tissues of the cardiovascular system, as well as skeletal muscles and kidneys. This means that stimulating hormones increase the rate and force of heart contractions.
Beta blockers serve as protection against atherosclerotic heart disease, relieving pain and preventing further development of the disease. The cardioprotective effect (protection of the heart) is associated with the ability of these drugs to reduce regression of the left ventricle of the heart and have an antiarrhythmic effect. They reduce pain in the heart area and reduce the frequency of angina attacks. But Beta blockers are not the best choice of drugs for treating hypertension unless the patient has complaints of chest pain and heart attacks.
Unfortunately, simultaneously with the blockade of beta-1 adrenergic receptors, beta-2 adrenergic receptors are also targeted, which there is no need to block. Because of this, negative side effects from taking medications occur. Beta blockers have serious side effects and contraindications. They are described in detail below in the article. The selectivity of a beta blocker is the extent to which a particular drug is able to block beta 1 adrenergic receptors without affecting beta 2 adrenergic receptors. All other things being equal, the higher the selectivity, the better, because there are fewer side effects.
Classification
Beta blockers are divided into:
- selective (cardioselective) and non-selective;
- lipophilic and hydrophilic, i.e. soluble in fats or water;
- There are beta blockers with and without intrinsic sympathomimetic activity.
We will consider all these characteristics in detail below. Now the main thing to understand is that There are 3 generations of beta blockers, and there will be more benefit if treated with a modern medicine, and not outdated. Because the effectiveness will be higher, and there will be much fewer harmful side effects.
Classification of beta blockers by generation (2008)
Third-generation beta blockers have additional vasodilating properties, i.e. the ability to relax blood vessels.
- When taking labetalol, this effect occurs because the drug blocks not only beta-adrenergic receptors, but also alpha-adrenergic receptors.
- Nebivolol increases the synthesis of nitric oxide (NO), a substance that regulates vascular relaxation.
- And carvedilol does both.
What are cardioselective beta blockers?
There are receptors in the tissues of the human body that respond to the hormones adrenaline and norepinephrine. Currently, alpha-1, alpha-2, beta-1 and beta-2 adrenergic receptors are distinguished. Recently, alpha-3 adrenergic receptors have also been described.
The location and significance of adrenergic receptors can be briefly presented as follows:
- alpha-1 - are localized in blood vessels, stimulation leads to their spasm and increased blood pressure.
- alpha-2 - are a “negative feedback loop” for the tissue regulation system. This means that their stimulation leads to a decrease in blood pressure.
- beta-1 - are localized in the heart, their stimulation leads to an increase in the frequency and strength of heart contractions, and also increases the myocardial oxygen demand and increases blood pressure. Also, beta-1 adrenergic receptors are present in large quantities in the kidneys.
- beta-2 - localized in the bronchi, stimulation causes relief of bronchospasm. These same receptors are located on liver cells; the effect of the hormone on them causes the conversion of glycogen into glucose and the release of glucose into the blood.
Cardioselective beta blockers are active primarily against beta-1 adrenergic receptors, rather than selective beta blockers, equally block both beta-1 and beta-2 adrenergic receptors. In the cardiac muscle, the ratio of beta-1 and beta-2 adrenergic receptors is 4:1, i.e., energetic stimulation of the heart is carried out mostly through beta-1 receptors. As the dosage of beta blockers increases, their specificity decreases, and then the selective drug blocks both receptors.
Selective and non-selective beta blockers reduce blood pressure approximately equally, but Cardioselective beta blockers have fewer side effects, they are easier to use for concomitant diseases. Thus, selective drugs are less likely to cause bronchospasm, since their activity will not affect beta-2 adrenergic receptors, which are located mostly in the lungs.
Cardio-selectivity of beta blockers: beta-1 and beta-2 adrenergic receptor blocking index
Selective beta-blockers are weaker than non-selective beta-blockers in increasing peripheral vascular resistance, so they are more often prescribed to patients with peripheral circulatory problems (for example, intermittent claudication). Please note that carvedilol (Coriol) is, although from the latest generation of beta blockers, not cardioselective. However, it is actively used by cardiologists, and the results are good. Carvedilol is rarely prescribed to lower blood pressure or treat arrhythmias. It is more often used to treat heart failure.
What is the intrinsic sympathomimetic activity of beta blockers?
Some beta blockers not only block beta adrenergic receptors, but also stimulate them. This is called the intrinsic sympathomimetic activity of some beta blockers. Drugs that have intrinsic sympathomimetic activity are characterized by the following properties:
- these beta blockers slow your heart rate to a lesser extent
- they do not significantly reduce the pumping function of the heart
- to a lesser extent increase total peripheral vascular resistance
- less likely to provoke atherosclerosis because they do not have a significant effect on blood cholesterol levels
You can find out which beta blockers have intrinsic sympathomimetic activity and which drugs do not.
If beta-blockers, which have intrinsic sympathomimetic activity, are taken for a long time, chronic stimulation of beta-adrenergic receptors occurs. This gradually leads to a decrease in their density in tissues. After this, suddenly stopping the medication does not cause withdrawal symptoms. At all, The dose of beta blockers should be reduced gradually: 2 times every 2-3 days for 10-14 days. Otherwise, serious withdrawal symptoms may appear: hypertensive crises, increased frequency of angina attacks, tachycardia, myocardial infarction or sudden death due to a heart attack.
Studies have shown that beta blockers, which have intrinsic sympathomimetic activity, are no different in their effectiveness in lowering blood pressure than drugs that do not have this activity. But in some cases, the use of drugs with internal sympathomimetic activity allows one to avoid unwanted side effects. Namely, bronchospasm with airway obstruction of various nature, as well as spasms in the cold with atherosclerosis of the vessels of the lower extremities. In recent years (July 2012), doctors have come to the conclusion that one should not attach much importance to whether a beta blocker has intrinsic sympathomimetic activity or not. Practice has shown that drugs with this property reduce the incidence of cardiovascular complications no more than those beta blockers that do not.
Lipophilic and hydrophilic beta blockers
Lipophilic beta blockers are soluble in fat, while hydrophilic beta blockers are soluble in water. Lipophilic drugs undergo significant “processing” during their initial passage through the liver. Hydrophilic beta-blockers are not metabolized in the liver. They are excreted from the body mainly in urine, unchanged. Hydrophilic beta blockers last longer because they are not eliminated as quickly as lipophilic beta blockers.
Lipophilic beta blockers penetrate the blood-brain barrier better. It is a physiological barrier between the circulatory system and the central nervous system. It protects nervous tissue from microorganisms, toxins and “agents” of the immune system circulating in the blood, which perceive brain tissue as foreign and attack it. Through the blood-brain barrier, nutrients enter the brain from the blood vessels, and waste products from the nervous tissue are removed back.
It turned out that lipophilic beta-blockers are more effective in reducing mortality in patients with coronary heart disease. At the same time, they cause more side effects from the central nervous system:
- depression;
- sleep disorders;
- headache.
In general, the activity of fat-soluble beta-blockers is not affected by food intake. It is advisable to take hydrophilic preparations before meals with plenty of water.
The drug bisoprolol is notable for its ability to dissolve in both water and lipids (fats). If the liver or kidneys are not working well, then the task of removing bisoprolol from the body is automatically taken over by the system that is healthier.
Modern beta blockers
- carvedilol (Ccoriol);
- bisoprolol (Concor, Biprol, Bisogamma);
- metoprolol succinate (Betaloc LOC);
- nebivolol (Nebilet, Binelol).
Other beta blockers can be used to treat hypertension. Doctors are recommended to prescribe second- or third-generation drugs to their patients. Above in the article you can find a table that describes which generation each drug belongs to.
Modern beta blockers reduce the likelihood of a patient dying from a stroke, and especially from a heart attack. At the same time, studies since 1998 have systematically shown that propranolol (anaprilin) not only does not reduce, but even increases mortality compared to placebo. There is also conflicting data on the effectiveness of atenolol. Dozens of articles in medical journals claim that it reduces the likelihood of cardiovascular “events” much less than other beta blockers, while causing more side effects.
Patients should understand that all beta blockers reduce blood pressure approximately equally. Perhaps nebivolol does this a little more effectively than everyone else, but not by much. At the same time, they reduce the likelihood of developing cardiovascular disease in very different ways. The main goal of treating hypertension is precisely to prevent its complications. It is assumed that Modern beta blockers are more effective in preventing complications of hypertension than previous generation medications. They are also better tolerated because they are less likely to cause side effects.
Back in the early 2000s, many patients could not afford to be treated with quality drugs because patented drugs were too expensive. But now you can buy generic drugs at the pharmacy, which are very affordable and still work effectively. Therefore, financial considerations are no longer a reason to avoid using modern beta blockers. The main task is to overcome the ignorance and conservatism of doctors. Doctors who do not follow the news often continue to prescribe old medications that are less effective and have significant side effects.
Indications for use
The main indications for the use of beta blockers in cardiological practice:
- arterial hypertension, including secondary (due to kidney damage, increased thyroid function, pregnancy and other reasons);
- heart failure;
- cardiac ischemia;
- arrhythmias (extrasystole, atrial fibrillation, etc.);
- long QT syndrome.
In addition, beta blockers are sometimes prescribed for vegetative crises, mitral valve prolapse, withdrawal syndrome, hypertrophic cardiomyopathy, migraine, aortic aneurysm, and Marfan syndrome.
In 2011, the results of a study of women with breast cancer who took beta blockers were published. It turned out that while taking beta blockers, metastases occur less frequently. The American study involved 1,400 women who had undergone surgery for breast cancer and were prescribed chemotherapy. These women were taking beta blockers because of cardiovascular problems they had in addition to breast cancer. After 3 years, 87% of them were alive and without cancer “events.”
The control group for comparison consisted of breast cancer patients of the same age and with the same percentage of patients with diabetes mellitus. They did not receive beta blockers and had a 77% survival rate. It is too early to draw any practical conclusions, but perhaps in 5-10 years beta blockers will become a simple and inexpensive way to improve the effectiveness of breast cancer treatment.
Use of beta blockers to treat hypertension
Beta blockers lower blood pressure generally as well as other classes of drugs. It is especially recommended to prescribe them for the treatment of hypertension in the following situations:
- Concomitant coronary heart disease
- Tachycardia
- Heart failure
- Hyperthyroidism is hyperfunction of the thyroid gland.
- Migraine
- Glaucoma
- Arterial hypertension before or after surgery
| Beta blocker drug name | Corporate (commercial) name | Daily dose, mg | How many times a day to take |
|---|---|---|---|
|
Cardioselective |
|||
|
Atenolol, atenobene, tenolol, tenormin | 25 - 100 | 1 - 2 |
|
Lokren | 5 - 40 | 1 |
|
Concor | 5 - 20 | 1 |
|
Vasocardin, Corvitol, Betaloc, Lopresor, Specicor, Egilok | 50 - 200 | 1 - 2 |
|
Nebilet | 2,5 - 5 | 1 |
|
Sectral | 200 - 1200 | 2 |
| Talinolol | Cordanum | 150 - 600 | 3 |
| Celiprolol | Celiprolol, selector | 200 - 400 | 1 |
|
Non-cardioselective |
|||
|
1. Beta blockers without intrinsic sympathomimetic activity |
|||
|
Korgard | 20 - 40 | 1 - 2 |
|
Anaprilin, obzidan, inderal | 20 - 160 | 2 - 3 |
|
Timohexal | 20 - 40 | 2 |
|
2. Beta blockers with intrinsic sympathomimetic activity |
|||
| Alprenolol | Aptin | 200 - 800 | 4 |
| Oxprenolol | Trazicore | 200 - 480 | 2 - 3 |
|
Betapresin, levatol | 20 - 80 | 1 |
|
Visken | 10 - 60 | 2 |
|
3. Beta blockers with alpha blocking activity |
|||
|
Coriol | 25 - 100 | 1 |
|
Albetol, normodin, trandate | 200 - 1200 | 2 |
Are these medications suitable for diabetes?
Treatment with “good old” beta blockers (propranolol, atenolol) can worsen tissue sensitivity to the effects of insulin, i.e. increase insulin resistance. If a patient is predisposed, his chances of developing diabetes increase. If the patient has already developed diabetes, its course will worsen. At the same time, when using cardioselective beta blockers, tissue sensitivity to insulin deteriorates to a lesser extent. And if you prescribe modern beta blockers, which relax blood vessels, then, as a rule, in moderate doses they do not disrupt carbohydrate metabolism and do not worsen the course of diabetes.
In 2005, the Kiev Institute of Cardiology named after Academician Strazhesko studied the effect of beta blockers on patients with metabolic syndrome and insulin resistance. It turned out that carvedilol, bisoprolol and nebivolol not only do not worsen, but even increase the sensitivity of tissues to the action of insulin. At the same time, atenolol significantly worsened insulin resistance. A 2010 study showed that carvedilol did not improve vascular insulin sensitivity, but metoprolol worsened it.
Patients may experience weight gain when taking beta blockers. This occurs due to increased insulin resistance, as well as other reasons. Beta blockers reduce metabolic rate and interfere with the process of breakdown of adipose tissue (inhibit lipolysis). In this sense, atenolol and metoprolol tartrate performed poorly. At the same time, according to research results, taking carvedilol, nebivolol and labetalol was not associated with a significant increase in body weight in patients.
Taking beta blockers may affect insulin secretion by the beta cells of the pancreas. These drugs can suppress the first phase of insulin secretion. As a result, the main tool for normalizing blood sugar is the second phase of insulin release by the pancreas.
Mechanisms of influence of beta blockers on glucose and lipid metabolism
| Index |
Treatment with non-selective or cardioselective beta blockers |
Metabolic consequences |
|---|---|---|
| Lipoprotein lipase activity | ? triglyceride clearance | |
| Lecithin-cholesterol acyltransferase activity | ? high density lipoproteins | |
| Body mass | ? insulin sensitivity | |
| Insulin secretion | ? Phase 2, prolonged hyperinsulinemia | |
| Insulin clearance | ? hyperinsulinemia, ? insulin resistance | |
| Peripheral blood flow | ? substrate delivery, ? glucose uptake | |
| General peripheral vascular resistance | ? peripheral blood flow |
Note to the table. It should be emphasized once again that modern beta blockers have a minimal negative effect on glucose and lipid metabolism.
In insulin-dependent diabetes mellitus, an important problem is that any beta blockers may mask symptoms of impending hypoglycemia- tachycardia, nervousness and trembling (tremor). At the same time, increased sweating continues. Also, diabetics who receive beta blockers have difficulty recovering from a hypoglycemic state. Because the main mechanisms of increasing blood glucose levels - glucagon secretion, glucogenolysis and gluconeogenesis - are blocked. However, in type 2 diabetes, hypoglycemia is rarely such a serious problem as to warrant treatment with beta blockers.
It is believed that if indicated (heart failure, arrhythmia and especially previous myocardial infarction) the use of modern beta blockers in patients with diabetes is advisable. In a 2003 study, beta blockers were prescribed to patients with heart failure and diabetes. The comparison group included patients with heart failure without diabetes. In the first group, mortality decreased by 16%, in the second - by 28%.
Diabetics are recommended to prescribe metoprolol succinate, bisoprolol, carvedilol, nebivolol - beta blockers with proven effectiveness. If the patient does not yet have diabetes, but is at increased risk of developing it, it is recommended to prescribe only selective beta blockers and not use them in combination with diuretics (water medications). It is advisable to use drugs that not only block beta-adrenergic receptors, but also have the properties of relaxing blood vessels.
Contraindications and side effects
Read the details in the article “”. Find out what contraindications exist for their use. Some clinical situations are not absolute contraindications for treatment with beta blockers, but require increased caution. You will find details in the article linked above.
Increased risk of impotence
Erectile dysfunction (complete or partial impotence in men) is what beta blockers are most often blamed for. It is believed that beta blockers and diuretics are groups of drugs for hypertension that most often lead to a deterioration in male potency. In reality, everything is not so simple. Research convincingly proves that new modern beta blockers do not affect potency. You will find a complete list of these drugs suitable for men in the article “”. Although old generation beta blockers (not cardioselective) can indeed worsen potency. Because they impair the blood supply to the penis and possibly interfere with the production of sex hormones. Nevertheless, Modern beta blockers help men control hypertension and heart problems while maintaining potency.
In 2003, the results of a study were published on the incidence of erectile dysfunction while taking beta blockers, depending on patient awareness. First, the men were divided into 3 groups. They were all taking a beta blocker. But the first group did not know what medicine they were being given. The men in the second group knew the name of the drug. For patients in the third group, doctors not only told them which beta blocker they were prescribed, but also informed them that decreased potency is a common side effect.

In the third group, the incidence of erectile dysfunction was the highest, as much as 30%. The less information patients received, the lower the frequency of potency weakening.
Then we carried out the second stage of the study. It involved men who complained of erectile dysfunction as a result of taking a beta blocker. They were all given another pill and told that it would improve their potency. Almost all participants noted an improvement in their erections, although only half of them were given real silendafil (Viagra), and the other half were given a placebo. The results of this study convincingly prove that the reasons for the weakening of potency while taking beta blockers are largely psychological.
In conclusion of the section “Beta blockers and increased risk of impotence”, I would like to once again urge men to study the article “”. It provides a list of modern beta blockers and other medications for hypertension that do not impair potency, and perhaps even improve it. After this, you will be much more comfortable taking blood pressure medications as prescribed by your doctor. It is foolish to refuse to be treated with beta blockers or other pills for hypertension for fear of worsening potency.
Why doctors are sometimes reluctant to prescribe beta blockers
Until recent years, doctors actively prescribed beta blockers to most patients who needed treatment for high blood pressure and prevention of cardiovascular complications. Beta blockers, together with the so-called old, or traditional, drugs for hypertension. This means that the effectiveness of new blood pressure-lowering tablets, which are constantly being developed and entering the pharmaceutical market, is compared with them. First of all, they are compared with beta blockers.
After 2008, publications appeared that beta blockers should not be the first choice drugs for the treatment of patients with hypertension. We will analyze the arguments that are given. Patients can study this material, but they should remember that the final decision on which medicine to choose remains with the doctor in any case. If you don't trust your doctor, just find another one. Make every effort to consult the most experienced doctor because your life depends on it.
So, opponents of the widespread therapeutic use of beta blockers argue that:
- These drugs are less effective than other hypertension medications in reducing the likelihood of cardiovascular complications.
- It is believed that beta blockers do not affect the stiffness of the arteries, that is, they do not stop, much less reverse, the development of atherosclerosis.
- These medications do little to protect target organs from the damage caused by high blood pressure.
There are also concerns that under the influence of beta blockers the metabolism of carbohydrates and fats is disrupted. As a result, the likelihood of developing type 2 diabetes mellitus increases, and if diabetes already exists, its course worsens. And that beta blockers cause side effects that impair the quality of life of patients. This refers, first of all, to a weakening of sexual potency in men. We discussed the topics “Beta blockers and diabetes” and “Increased risk of impotence” in detail above in the relevant sections of this article.
There have been studies that show that beta blockers are worse than other hypertension medications at reducing the risk of cardiovascular complications. Relevant publications in medical journals began to appear after 1998. At the same time, there is evidence from an even larger number of reliable studies that have obtained opposite results. They confirm that all major classes of blood pressure-lowering drugs have approximately the same effectiveness. The generally accepted view today is that Beta blockers are very effective after a myocardial infarction to reduce the risk of recurrent infarction. As for prescribing beta blockers for hypertension to prevent cardiovascular complications, each doctor makes his own opinion based on the results of his practical work.

If the patient has severe atherosclerosis or a high risk of atherosclerosis (see what tests need to be taken to find out), then the doctor should pay attention to modern beta blockers, which have vasodilation properties, i.e., relax blood vessels. It is the blood vessels that are one of the most important target organs that are affected by hypertension. Among people who die from cardiovascular diseases, in 90% it is vascular damage that leads to death, while the heart remains absolutely healthy.
What indicator characterizes the degree and rate of development of atherosclerosis? This is an increase in the thickness of the intima-media complex (IMC) of the carotid arteries. Regular measurement of this value using ultrasound serves to diagnose vascular damage both as a result of atherosclerosis and due to hypertension. With age, the thickness of the inner and middle linings of the arteries increases; this is one of the markers of human aging. Under the influence of arterial hypertension, this process is much accelerated. But under the influence of medications that lower blood pressure, it can slow down and even reverse. In 2005, a small study was conducted on the effect of taking beta blockers on the progression of atherosclerosis. Its participants included 128 patients. After 12 months of taking the drug, a decrease in intima-media thickness was observed in 48% of patients treated with carvedilol and in 18% of those treated with metoprolol. Carvedilol is believed to be able to stabilize atherosclerotic plaques due to its antioxidant and anti-inflammatory effects.
Features of prescribing beta blockers to elderly people
Doctors are often wary of prescribing beta blockers to older people. Because this “complex” category of patients, in addition to heart and blood pressure problems, often have concomitant diseases. Beta blockers may worsen their course. Above we discussed how drugs from the beta blocker group affect the course of diabetes. We also recommend to your attention a separate article “”. The practical situation now is that beta blockers are prescribed 2 times less often to patients over 70 years of age than to younger ones.
With the advent of modern beta blockers, side effects from their use have become much less common. Therefore, “official” recommendations now indicate that beta blockers can be more safely prescribed to older patients. Studies from 2001 and 2004 showed that bisoprolol and metoprolol succinate reduced mortality equally in younger and older patients with heart failure. In 2006, a study of carvedilol was conducted, which confirmed its high effectiveness in heart failure and good tolerability in elderly patients.

Thus, if there is evidence, then beta blockers can and should be prescribed to elderly patients. In this case, it is recommended to start taking the medication with small doses. If possible, it is advisable to continue treatment of elderly patients with low doses of beta blockers. If there is a need to increase the dose, this should be done slowly and carefully. We recommend to your attention the articles “” and “”.
Can hypertension be treated with beta blockers during pregnancy?
What is the best beta blocker?
There are a lot of beta blocker drugs. It seems that each drug manufacturer produces its own tablets. This can make it difficult to choose the right medication. All beta blockers have approximately the same effect on lowering blood pressure, but they differ significantly in their ability to prolong the life of patients and the severity of side effects.
The doctor always chooses which beta blocker to prescribe! If the patient does not trust his doctor, then he should consult another specialist. We strongly discourage self-medication with beta blockers. Re-read the article “” again and make sure that these are not harmless pills, and therefore self-medication can cause great harm. Make every effort to be treated by the best doctor. This is the most important thing you can do to prolong your life.
The following considerations will help you choose a medicine together with your doctor (!!!):
- For patients with underlying kidney problems, lipophilic beta blockers are preferred.
- If the patient has liver disease, most likely, in this situation the doctor will prescribe a hydrophilic beta blocker. Specify in the instructions how the drug you are going to take (prescribe to the patient) is eliminated from the body.
- Old beta blockers often impair potency in men, but modern drugs do not have this unpleasant side effect. In the article ““ you will find out all the necessary details.
- There are drugs that act quickly, but not for long. They are used for hypertensive crises (labetalol intravenously). Most beta blockers do not begin to act immediately, but lower blood pressure over a long period of time and more gradually.
- It is important how many times a day you need to take this or that drug. The less, the more convenient it is for the patient, and the less likely he is to quit treatment.
- It is preferable to prescribe new generation beta blockers. They are more expensive, but have significant advantages. Namely, it is enough to take them once a day, they cause a minimum of side effects, are well tolerated by patients, do not worsen glucose metabolism and lipid levels in the blood, as well as potency in men.
Doctors who continue to prescribe the beta blocker propranolol (Anaprilin) deserve condemnation. This is an outdated drug. It has been proven that propranolol (anaprilin) not only does not reduce, but even increases the mortality of patients. It is also controversial whether it is worth continuing to use atenolol. In 2004, the prestigious British medical journal Lancet published an article “Atenolol for hypertension: is it a wise choice?” It stated that the prescription of atenolol was not an appropriate medication for the treatment of hypertension. Because it reduces the risk of cardiovascular complications, but does it worse than other beta blockers, as well as blood pressure medications from other groups.
You can find out which specific beta blockers are recommended earlier in this article:
- to treat heart failure and reduce the risk of sudden death from heart attack;
- men who want to lower blood pressure, but are afraid of deterioration in potency;
- diabetics and those at increased risk of diabetes;
We remind you once again that the final choice of which beta blocker to prescribe is made only by the doctor. Don't self-medicate! The financial side of the issue should also be mentioned. A lot of pharmaceutical companies produce beta blockers. They compete with each other, so the prices for these drugs are quite affordable. Treatment with a modern beta blocker will most likely cost the patient no more than $8-10 per month. Thus, the price of a drug is no longer a reason to use an outdated beta blocker.
Beta blockers are medications that block natural processes in the body. In particular, stimulation of the heart muscle with adrenaline and other “accelerating” hormones. It has been proven that these drugs in many cases can extend the patient's life by several years. But they have no effect on the causes of hypertension and cardiovascular diseases. We recommend to your attention the article “”. Magnesium deficiency in the body is one of the common causes of hypertension, heart rhythm disturbances and blockage of blood vessels with blood clots. We recommend. They eliminate magnesium deficiency and, unlike “chemical” drugs, truly help lower blood pressure and improve heart function.

For hypertension, in second place after magnesium is hawthorn extract, followed by the amino acid taurine and good old fish oil. These are natural substances that are naturally present in the body. Therefore, you will experience “side effects” from , and they will all be beneficial. Your sleep will improve, your nervous system will become calmer, swelling will go away, and in women, PMS symptoms will become much easier.
For heart problems, it comes in second place after magnesium. This is a substance that is present in every cell of our body. Coenzyme Q10 is involved in energy production reactions. In the tissues of the heart muscle its concentration is twice as high as the average. This is a phenomenally useful remedy for any heart problems. To the point that taking coenzyme Q10 helps patients avoid a heart transplant and live normally without it. Official medicine has finally recognized coenzyme Q10 as a cure for cardiovascular diseases. Registered and . This could have been done 30 years ago, because progressive cardiologists have been prescribing Q10 to their patients since the 1970s. I would especially like to note that Coenzyme Q10 improves survival of patients after a heart attack, i.e., in the same situations where beta blockers are especially often prescribed.
We recommend that patients start taking a beta blocker as prescribed by their doctor along with natural health benefits for hypertension and heart disease. At the beginning of treatment, do not try to replace the beta blocker with any “folk” methods of treatment! You may be at high risk of having a first or second heart attack. In such a situation, the medicine truly saves you from sudden death due to a heart attack. Later, after a few weeks, when you feel better, you can carefully reduce the dosage of the medicine. This should be done under the supervision of a doctor. The ultimate goal is to stay completely on natural supplements, instead of “chemical” pills. With the help of the materials on our site, thousands of people have already been able to do this, and they are very pleased with the results of this treatment. Now you.
Articles in medical journals on the treatment of hypertension and cardiovascular disease with CoQ10 and magnesium
| No. | Article title | Magazine | Note |
|---|---|---|---|
| 1 | The use of coenzyme Q10 in complex therapy of arterial hypertension | Russian Journal of Cardiology, No. 5/2011 | |
| 2 | Possibilities of using ubiquinone in the treatment of arterial hypertension | Russian Journal of Cardiology, No. 4/2010 | Ubiquinone is one of the names of coenzyme Q10 |
| 3 | Magnesium in the treatment and prevention of cerebrovascular diseases | Cardiology, No. 9/2012 | |
| 4 | The use of magnesium in cardiovascular diseases (chronic coronary syndrome, arterial hypertension and heart failure) | Russian Journal of Cardiology, No. 2/2003 | |
| 5 | The use of magnesium in cardiological practice | Russian Journal of Cardiology, No. 2/2012 | The drug Magnerot is being discussed. We recommend other magnesium supplements that are just as effective but cheaper. |
| 6 | Potassium and magnesium deficiency as a risk factor for the development of cardiovascular diseases | Russian Medical Journal, No. 5, February 27, 2013, “Man and Medicine” |
Any modern cardiologist knows how beneficial magnesium, fish oil and coenzyme Q10 are for the heart. Tell your doctor that you will be taking a beta blocker along with these supplements. If the doctor objects. - it means that he is behind the times, and it is better for you to turn to another specialist.
- Olga
Is it necessary to take blockers for neurosis?
- Tamara
I am 62 years old, height 158, weight 82. The pressure persists for the second week, tachycardia. I drink, lozap 2 times (50 and 25 mg), ogelok (25 mg), amlotop (2.5), but there is no stabilization of pressure. Is it possible to change medications?
- Anton
how Q10 can replace beta blockers
after all, they take the load off the heart during angina, and Q10 is just a vitamin - Stas
51 years old 186 cm. 127 kg-
atrial fibrillation. dry mouth. nocturnal polyuria - more than 1 liter of urine. Diabetes is not diagnosed. Sugar levels are normal in the morning. I’m on a diet. If you eat something sweet after 6 or just eat something in the evening, you get excited. insomnia. From 12 at night to 4 in the morning there was an urge to go to the toilet, which led to a disruption of the rhythm. This has been going on for many years. I accept Valz and Egilok. During the day, the bladder does not bother The adrenal glands are normal Blood tests are normal No sexual infections have been detected Can Egilok reduce the production of antidiuretic hormone? Does it make sense to change it to Concor? (I tried it once, but migraines started) Thanks - Natalia
45 years old, height 167, weight 105 kg. Bisoprolol 2.5 mg was prescribed for the first time. The pressure fluctuates, but not higher than 140/90. How long should I use it, my whole life?
- Andrey
51 years old, 189 cm, 117 kg.
Six years ago, the doctor prescribed Noliprel blood pressure 200/100.
At the moment, after coughing symptoms, I stopped taking medications; my blood pressure was 160/100.
After the examination, the doctor prescribed Valsacor 160, biprol 5 mg, Arifon retard 1.5 mg, Atoris 20 mg.
The pressure became 110/70.
Is it worth taking this set of medications? - Vadim
I am 48 years old, height 186, weight 90 kg. I was diagnosed with hypertension at the age of 16, for the last 5 years I have been taking Locrene 5 mg once a day, the upper pressure does not rise above 130, and the lower one is often 95-100, I have also become weather-sensitive, and lately I have had poor sleep, anxiety , deterioration in sex life (poor erection) I live in a village, the doctors are far from me, I have two questions: do I need to look for a replacement for Lokren and can I sometimes take Viagra or other drugs to improve erection, thank you
- Galina
58 years /168cm /75kg
working pressure is 140/90, periodically jumps to 170/100, but the main thing is that the pulse is constantly 90 and higher, even after sleep it feels like I’ve run 100 meters; Sugar and cholesterol are normal, I smoke, my diet is average (I allow fatty foods), an ultrasound showed excess fat on the liver. I periodically take anaprilin (when my pulse goes through the roof). Now the doctor prescribed bisoprolol. Should I start taking it or try to do without chemicals first? - Igor
26 years old, 192cm, weight 103. I went to the doctor with tachycardia 90-100 beats/min and he prescribed me bisoprolol 5 mg per day. I work out in the gym and cycle. Can I continue training?
- admin Post author
> 26 years old, 192cm, weight 103. See a doctor
> with tachycardia 90-100 beats/minI explain how to determine your normal heart rate. The theoretical maximum is 220 beats per minute minus age, i.e. for you 194 beats per minute. The resting pulse is about 50% of the maximum, i.e. for you 82 plus or minus 10 beats per minute. Even with light loads, the heart rate rises to 55-65% of the theoretical maximum.
Conclusion: if you feel normal, then you have no trace of tachycardia. But if you feel bad, then this is the second question...
> is it possible to continue training?
Depends on how you feel.
If I were you, I would now do the following:
1. Read the list of references here -
2. Books “Younger Every Year” and “Chi-Running. A revolutionary way to run" - you can easily find it if you want.
3. From the book “Younger Every Year” you will learn a lot of interesting things about the pulse
4. You are overweight - study our articles in the block “Cure from hypertension in 3 weeks - it’s real” and now switch to a low-carbohydrate diet. If you do this from a young age, then in adulthood you will not have the problems that your peers will have, and they will envy your health.
5. Buy a heart rate monitor and train with it.> he prescribed me bisoprolol 5 mg per day
If you feel normal, then you don’t need bisoprolol for nothing. And if there are complaints about the heart, then you need to be thoroughly examined, and not just “suppress” the symptoms with chemical tablets.
- Igor
Thanks for the answer. The complaint about my heart is that I feel it beating and at the same time there are also arrhythmias that cause discomfort. The main problem is that I am easily excitable, at the slightest stress adrenaline is released and the pulse instantly rises to 110. I did a cardiogram, the doctor said that there is dystrophy myocardium, but this is not serious and many people have this. 7 years ago I had stage 1 fibrosis of the mitral valve. I’ll go do an ultrasound and see what’s there now. Today I took a biprolol tablet and I felt much better, my pulse is 70, like an astronaut's :-) though this is not an option and I understand that. We need to get examined. As for the pressure, it happens that it rises to 140, but I would not say that this is my problem. The pressure can only play out once a month or even less often.
- Igor
- admin Post author
- Natalia
Please tell me, is it possible to take Nebilet when planning a pregnancy, does it affect conception?
My husband and I take this drug, the doctor thinks it is necessary... - yagut
Hello, what antihypertensive medication would you recommend for a patient taking chemotherapy? A/D 190/100, P/s 102 min.
- Tatiana
Hello. Mom is 80 years old. Diagnosis: hypertension with predominant heart damage. With heart failure ||st. WHO, 3st. Dyslepidemia||A according to Fredrickson.NK ||f.k (NYHA). LVDD. relative mitral regurgitation. Episodes of sinus tachycardia. Dyscirculatory encephalopathy grade 2 of complex origin (hypertensive, atherosclerotic). Significant stenosis of the right vertebral artery. Parapervical cyst of the left kidney. Prescribed: ramipril 2.5-5.0 mg in the morning, betaloc zok 25 mg in the morning, amlodipine 5 mg in the evening. The problem is that mom feels very bad, pressure surges, night tremors and shudders and a sharp increase in pressure, feelings of anxiety and fear, severe cough and dry throat. Noise in the head and knocking. Tell me whether the treatment has been prescribed correctly, is it possible to replace Betaloc with another beta blocker (as it has a strong side effect in the form of coughing attacks and shortness of breath). Mom's height is 155, weight 58 kg.
- admin Post author
Is it possible to replace Betaloc with another beta blocker?
Discuss this issue with your doctor, but this is unlikely to make sense
severe side effects in the form of coughing attacks and shortness of breath
I suspect that taking other beta blockers will do the same. The patient is 80 years old, her body is worn out... nothing surprising. Perhaps the doctor will decide to stop the beta blocker altogether, since the patient tolerates them so poorly. But don’t cancel it yourself, it can lead to a sudden heart attack.
If I were you, I would no longer expect a miracle from any treatment. Read the article ““. Try adding magnesium-B6 to your mother, as prescribed there, along with the medications prescribed by the doctor. In no case instead of medications, but in addition to them.
pressure surges, night tremors and shudders, feelings of anxiety and fear
There is a chance that these symptoms will improve as a result of taking magnesium.
If finances allow, then try Coenzyme Q10.
- Tatiana
I want to ask you, amlodipine, my mother was prescribed to take it in the evening, what time is the best time to take it in the evening? If she drinks it at 9 p.m., her blood pressure will definitely jump. And it turns out to be a vicious circle: the medicine seems to be helping, but a surge in pressure occurs. Thank you.
- admin Post author
>it seems like the medicine should
>help, but there is a pressure surgeI would suggest skipping the medication once and seeing how your blood pressure behaves in response. But in your case, this risks a heart attack or stroke. So I don’t recommend taking risks.
- admin Post author
- Tatiana
- admin Post author
- Catherine
Hello, I am 35 years old, height 173, weight 97 kg. I am 13 weeks pregnant, I had stage 2 hypertension before pregnancy and now my blood pressure is rising to 150/100 due to medications. Today my pulse was 150, I was afraid that I might have a stroke or my heart would break. Can pregnant women take beta blockers? Gynecologists disagree.
- Tatyana Iosifovna
Dear doctor! I am 73 years old. I have had hypertension since I was 50. I had a mastectomy of the mammary gland 2 years ago. I am being monitored. There are no special complaints from oncology. Problems with blood vessels. In the morning the pressure is either low or normal. There is no tachycardia. Emergency - 65-70.
I was prescribed Betaloc, Cardiomagnyl and Lazap Plus.
The beta blocker should be taken in the morning. But with a heart rate of 60, I hesitate to take it. The pressure rises (to 170) in the second half of the day. At the same time, it is not always relieved by taking antihypertensive drugs, tachycardia develops (up to 95-98). To reduce pressure, I take another 15-20 mg of Physitenza before bed. The pressure normalizes, but the heart rate does not. There are feelings of constriction in the heart area.
ECG: SR not excluded. c/o changes in the basal parts of the left ventricle.
ECHO:LVH of the basal part of the IVS, type DD2. Chambers and valves are normal.
Question: when is the best time to take beta blockers? They also lower blood pressure. I have a hard time with hypotension; Shortness of breath appears both when walking and lying down. In the morning I feel normal.
P.S. my height is 164, weight is 78 kg. Sincerely, T.I. - Dmitriy
Dear doctor, help me figure it out so I can understand exactly what is happening to me. City of Kiev, height 193, weight 116 kg, waist circumference 102 cm. In August 2013, there was a reason to call an ambulance, it all happened on Monday at lunchtime on the street (heat), sudden weakness, dizziness, fear of falling, then I felt panic, palpitations . They called an ambulance, my blood pressure was 140/100, my pulse was 190. They injected me with something and gave me anaprilin under my tongue and Corvalol. After this, I went to the doctors, took blood tests, the blood showed glucose 7.26, liver tests of ALT and AST were significantly elevated. They attributed it to the fact that there had been alcoholic libations before and subsequent poisoning. They did an ultrasound of the heart, a cardiogram, then a gastroscopy at the Shalimov Institute, an MRI (they found glaucoma, all other organs were OK), in general, almost all the tests. They told me to drink bisoprolol 5 mg every day. A diagnosis of stage 1 hypertension was made. They recommended a lifestyle change, diet, walking, giving up alcohol. I took bisoprolol for 2 months, the pressure stabilized immediately - it was always normal, then somewhere after 1.5 months bisoprolol began to lower the pressure 105-115/65-75, the dose was reduced. Then I felt great and had a cardiogram done on a cardio machine under different loads. The doctor said based on the results that there is nothing to complain about the heart, everything is OK, we are canceling bisoprolol. Bisoprolol was abruptly stopped; I took 2.5 mg for the last 2 weeks. And then it began - in almost two weeks, three attacks, heart rate jumps to 100 and above, with subsequent pressure jumps to 150/95. Knocked down and calmed down with Corvalol. Fears began that this might happen again. I turned to the same cardiologist - again bisoprolol 2.5 mg for the winter and consult a neurologist. The latter prescribed the anti-depressant Triticco, which was supposed to relieve fears, panic, etc. When they were taken together, the pressure in the cold remained stable at 118-124/65-85, and then the pressure dropped again to 105/60. The neurologist again abruptly stopped bisoprolol. The situation appeared again, twice in 4 days - incomprehensible anxiety, rapid pulse above 100, and probably blood pressure. I already knocked it down with Corvalol and anaprilin. After this, the fears resumed, the cardiologist advised Nebilet, which lowers the blood pressure less and keeps the pulse better than bisoprolol. Don’t quit Tritiko and finish it, and also, to somehow knock bad thoughts out of your head, take gedozepam. I don’t understand what to do next, where to go? Your site is very informative, but it’s difficult to find doctors even in Kyiv. They say that the problem is in my head, I create my own fears. Please advise, sometimes it seems to me that my doctors have no time for me. Age 45 years.
Treatment of hypertension without drugs."
- Dmitriy
Thank you very much for your answer. I did not write (missed) that after I was tested for the first time (which showed glucose 7.26), and this was 08.20.13, I stopped drinking alcohol, began taking bisoprolol, taking walks, and eating selectively. A week later, namely 08/28/13, I donated blood again at Shalimov’s clinic and my glucose showed 4.26. With this, I calmed down regarding sugar (the doctors attributed the cause of the crisis and high blood glucose to the fact that a week before there was severe alcohol poisoning at a birthday party). As I understand it, we urgently need to take all the tests again in the order that you recommend, and follow the recommendations on the website - diet, exercise, that’s 100%. What about my pulse jumps, panic attacks? Or do you think they are closely related to glucose? As of today, I have stopped taking my own antidepressant and am again taking bisoprolol instead of Nebilet. It is much easier on bisoprolol, although panic attacks appear during the day. What do you recommend doing about this? Is it possible to cope with panic attacks and stop bisoprolol after some time if it turns out that my glucose levels are okay?
- Dmitriy
Good afternoon I am 65 years old, height 175 cm, weight 85 kg. Hypertension began to appear about 7 years ago. Previously, the pressure did not rise above 140, but I suffered with a very severe headache in the back of the head on the right. I started taking various medications. We went with the doctor for Lozap and Lerkamen, I took it for 2-3 years. But a crisis occurred, the pressure was 200, and Valsacor and Azomex were now prescribed. But I don’t feel well, in the morning the pressure is 130-140, in the afternoon 115, in the evening 125 and all the time my pulse is high from 77 to 100. My heart “aches”, it presses. I consulted other doctors, did all sorts of tests - there were no significant deviations. One doctor actually said that I don’t have any hypertension, I need to take sedatives. An ultrasound of the heart makes a diagnosis of stage 2 hypertension. I ask for your advice. Sincerely, Tatyana Grigorievna.
Hello. I am 37 years old, height 165 cm, weight 70 kg. Pulse 100-110 at rest, blood pressure 100-110/70. In 1993, she underwent surgery for nodular goiter. It was then, at the age of 16, that they told me that I had severe tachycardia. Since then I have known that it exists. True, I can’t say that it particularly bothers me if I’m in a calm state. With physical activity, I can hear my heart beating and ready to jump out of my chest. What worries me is rather the doctors, who say that this is not normal, that the heart wears out faster, and prescribe anaprilin, which I don’t want to take. Among other things, it also reduces blood pressure. But doctors don’t find the reasons as such (or don’t know what and where to look). At the same time, according to ultrasound of the heart, there was mitral valve prolapse of the 2nd degree. Decoding the daily holter didn’t tell the doctor anything either. I am registered with an endocrinologist and regularly do control ultrasounds and T3, T4, TSH. According to the endocrinologist, everything is normal. I have not been prescribed hormonal therapy, i.e. the thyroid gland is not the cause of tachycardia. At my last visit to the cardiologist, I was offered the option of prescribing beta blockers. True, the doctor asked me if I was still going to get pregnant? I said that I did not exclude this possibility, and then the doctor rejected the question of beta blockers for now. And that’s it - he didn’t prescribe anything else. But at the same time he again mentioned that the pulse was too high. With that we said goodbye. What to do?
The doctor prescribed me obzidan 3 times a day for tachycardia. At the pharmacy, before purchasing, I read the instructions and, after reading the list of side effects, decided to refuse the purchase. After about a month, I finally decided to buy the medicine, because the tachycardia was making itself felt, the pulse was 100-120. I didn’t find the paper with the name of the medicine, and I didn’t remember it by heart. I read about bisoprolol on the Internet. I decided to try it. At first I took 2.5 mg per day, then 5 mg. At first my limbs were frozen and I felt weak (side effects of bisoprolol), but then it seemed normal. Now I found a paper with the name - obzidan. Should I change bisoprolol to obzidan? Moreover, bisoprolol helps me and it is selective. After reading the article, I decided that there was no need to change bisoprolol. What do you think? Thank you. Andrey. 22 years old, height 176, weight 55 (yes, I’m skinny), blood pressure 120/80. Yes, even if I forget to take a bisoprolol tablet, the previous tablet is valid for another 1-1.5 days (2.5 days in total). And there is no obsidian for sure.
Hereditary hypertension, I have been suffering since I was 33 years old. Jumps in blood pressure are accompanied by nosebleeds. The drug combinations were changed. I used to take Concor and Valz twice a day, then they changed the combination to Nebilet, Arifon, Noliprel Bi Forte. In the morning and evening the pressure is almost always 150-160/90, during the day it drops to 130-140/80-90.
Two weeks ago they replaced it with the combination: Betaloc ZOK + Micardis plus. There is no special effect. Pressure is within 150-160/90. The scheme doesn't work. I am inclined to return to the previous option, but I need a third drug at night. I have read the recommendations above and hope for your advice.
Thank you!!!
Hello! My weight is 108.8 kg, I’m losing weight, 1.5 months ago I weighed 115 kg. Age 40 years. I have had hypertensive crises for 15 years—pressure surges from 130 to 170/97/95 and pure white urine discharge after a crisis. The limbs get cold and sweat, the heartbeat quickens - the pulse ranges from 80 to 115. In such cases I take anaprilin. If there is a severe crisis, I can add 40 drops of Valocordin - after 30 minutes everything calms down, I feel great. Only recently I had a crisis, I took Anaprilin and 40 drops of Valocordin. I called an ambulance and while it was on its way, everything was restored. I was happy, but 30 minutes later the same crisis hit me again. I went to the hospital emergency room - they put me in therapy, but didn’t give me any pills. By evening the pressure recovered on its own, leaving only a mild headache in the right back of the head. While I was in the hospital for examination, I took many tests - nothing was found. I took tablets Noliprel, Piracetam, Cytoflavin, sodium chloride, amitriptyline, Meloxicam. 10 days later, right on the doctors’ round, a crisis began - the pulse was 140, I thought my heart would jump out of my chest, the pressure was 170. I asked the nurse to give me anaprilin urgently - she said that the doctor was on rounds, and without it I wouldn’t give anything. But I’m getting worse... I asked to call a doctor, to which they said - go to the room and wait for the doctor. He came about 10 minutes later. It was hard for me, my legs began to shake. They gave me an injection, gave me Enap, anaprilin and 40 drops of Valocordin, I lay down for 30-40 minutes - I felt better, my blood pressure remained at 140. They took a cardiogram - they said everything was fine. They put on a Sibazol drip - after 10 minutes I was like a cucumber. Upon discharge, the doctor said and gave me an extract that I need to drink Bisoprolol every day. Now it’s been 3 months of drinking it, I felt good, there were no problems with blood pressure. For some reason, a week ago there was another crisis. True, I reduced the dose of Bisoprolol - I divided the tablet in half. Question: should I continue taking Bisoprolol or stop taking it? Should I fight this disease as before with anaprilin? These crises can occur at different times. At first, a slight trembling is felt, then the tips of the fingers become cold, cold sweat appears on the palms and feet, and pressure increases. The doctor said that we need to look for the cause of hypertension and get tested for metonephrines. Unfortunately, they don’t do it in our city. I'll be on vacation on the mainland - what should I do to check for this disease and how can I get rid of it? I’m so tired of taking these pills, I want to forget about them. I don’t smoke, I don’t drink alcohol, although sometimes I crave cognac. Thank you for the answer!
Hello. I am 18 years old, height 156 cm, weight 54 kg.
It all started with the fact that I experienced stress in the summer after graduation, and also entering a university had a significant impact on my health. I had neurosis and blood pressure up to 130/90. On the night of my birthday (I was running back and forth all day), I had a panic attack and my blood pressure rose to 140. Two cardiologists prescribed bisangyl and diagnosed VSD of the hypertensive type. I have been taking this medicine for a month and a half. The cardiologist said that the dose can be reduced. I took 0.5 bisangyl tablets for 10 days, and then stopped - and I developed heat in my cheeks, tremors in my hands, and tachycardia. There was no tonometer nearby, so I couldn’t measure the pressure. At the university they took my blood pressure - 142/105, pulse 120. I drank bisangil - and my blood pressure dropped to 110. What could have caused this?
Hello. I am 63 years old, height 171 cm, weight 65 kg. The CABG operation was performed in March 2015.
I constantly take Aspecard or Cardiomagnil 75 mg, Rosucard 5 mg and also Preductal intermittently. I can handle loads well. Recently, a permanent blockade of the right leg appeared, a course of treatment removed it. Bradycardia - pulse up to 45 beats/min, more often in the morning. Blood pressure 105-140/60-80. Sometimes arrhythmia appears after exercise.
Question: Doctors constantly prescribe at least small doses of beta blockers - bisoprolol, carvidex. I took 1.25 mg. As a rule, pressure drops to 105/65 and heart rate to 50-60. And I stop taking them. How important are beta blockers in my case?
Thank you.
Hello! I am 31 years old, height 180 cm, weight 68 kg.
I have experienced attacks of extrasystole since my youth. In the last few months, the extrasystoles have become very disturbing, once I had a panic attack - I turned to a cardiologist. Pulse is always 75-85.
According to Holter, 2300 ventricular extrasystoles per day. Ultrasound of the heart revealed fibrotic changes in the mitral valve. Ultrasound of the thyroid gland - 0.5 cm nodule in the left lobe. TSH, T4 and cholesterol are normal. The pressure is always normal.
The cardiologist prescribed Biol 0.25 mg, Panangin and Tenoten. In the first week of taking Biol, the pulse decreased and the sensations of interruptions in the heart disappeared. Then it began to increase again, now the average is 80 beats/min. Sometimes I feel interruptions in my heartbeat, a constant feeling of heaviness in the area of the heart, radiating to my left arm, I began to have very difficulty falling asleep, I have nightmares, I wake up with a feeling of fear, and I have shortness of breath.
When prescribing, the doctor did not even ask about possible pregnancy. We are planning a child, but after reading the reviews, I am now afraid to stop taking this drug.
Didn't find the information you were looking for?
Ask your question here.
How to cure hypertension on your own
in 3 weeks, without expensive harmful drugs,
"starvation" diet and heavy physical training:
free step-by-step instructions.
or, conversely, criticize the quality of site materials
For more than 20 years, beta-blockers have been considered one of the main drugs in the treatment of heart diseases. Scientific studies have obtained convincing data that served as the basis for including this group of drugs in modern recommendations and protocols for the treatment of cardiac pathologies.
Blockers are classified depending on their mechanism of action, which is based on the influence of a certain type of receptor. Today there are three groups:
- alpha-blockers;
- beta blockers;
- alpha-beta adrenergic blockers.
Alpha blockers
Drugs whose action is aimed at blocking alpha-adrenergic receptors are called alpha-blockers. The main clinical effects are dilation of blood vessels and, as a result, a decrease in total peripheral vascular resistance. This is followed by relief of blood flow and reduction of pressure.
In addition, they are able to lower cholesterol levels in the blood and influence fat metabolism in the body.
Beta blockers
There are different subtypes of beta-adrenergic receptors. Depending on this, beta blockers are divided into groups:
- Selective, which, in turn, are divided into 2 types: those with internal sympathomimetic activity and those without;
- Non-selective - block both beta-1 and beta-2 receptors;
Alpha-beta blockers
Representatives of this group of drugs reduce systole and diastole and heart rate. One of their main advantages is the lack of influence on the blood circulation of the kidneys and peripheral vascular resistance.
Mechanism of action of adrenergic blockers
Due to this, blood from the left ventricle, when the myocardium contracts, immediately enters the largest vessel of the body - the aorta. This point is important when the functioning of the heart is impaired. When taking these medications with combined action, there is no negative effect on the myocardium and, as a result, mortality is reduced.
General characteristics of ß-blockers
Beta-adrenergic receptor blockers are a large group of drugs that have the properties of competitively (reversibly) and selectively inhibiting the binding of catecholamines to the receptors of the same name. This group of drugs began to exist in 1963.
Then the drug Propranolol was synthesized, which is still in wide clinical use today. Its creators were awarded the Nobel Prize. Since that time, a number of drugs with adrenergic blocking properties have been synthesized, which had a similar chemical structure, but differed in some characteristics.

Properties of beta blockers
In a very short time, beta-blockers have taken a leading place in the treatment of most cardiovascular diseases. But if we go back into history, not so long ago the attitude towards these medications was slightly skeptical. First of all, this is due to the misconception that medications can reduce the contractility of the heart, and beta blockers were rarely used for diseases of the cardiac system.
However, today their negative effect on the myocardium has been refuted and it has been proven that with constant use of adrenergic blockers, the clinical picture changes dramatically: the stroke volume of the heart and its tolerance to physical activity increases.
The mechanism of action of beta-blockers is quite simple: the active substance, penetrating into the blood, first recognizes and then captures the molecules of adrenaline and norepinephrine. These are hormones synthesized in the adrenal medulla. What happens next? Molecular signals from the captured hormones are transmitted to the corresponding cells of the organs.
There are 2 main types of beta-adrenergic receptors:

Both receptors are present in the organocomplex of the central nervous system. There is also another classification of adrenergic blockers depending on their ability to dissolve in water or fat:

Indications and restrictions
The area of medical science in which beta blockers are used is quite wide. They are used in the treatment of many cardiovascular and other diseases.
The most common indications for the use of these drugs:
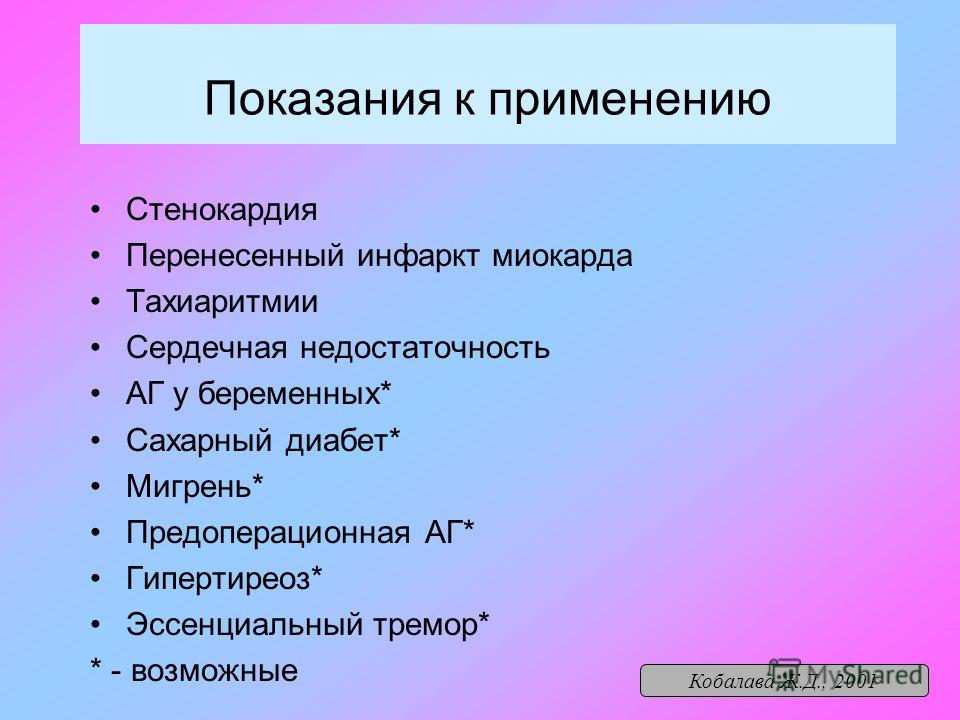
Disputes about when drugs of this group can be used and when not continue to this day. The list of diseases for which the use of these substances is not advisable is changing, as scientific research is constantly underway and new medications from the group of beta blockers are being synthesized.
Therefore, a conventional line has been defined between absolute (when it should never be used) and relative (when there is little risk) indications for the use of beta blockers. If in some sources certain contraindications are considered absolute, then in others they are relative.
 According to clinical protocols for the treatment of cardiac patients, it is strictly forbidden to use blockers when:
According to clinical protocols for the treatment of cardiac patients, it is strictly forbidden to use blockers when:
- severe bradycardia;
- high degree atrioventricular block;
- cardiogenic shock;
- severe lesions of peripheral arteries;
- individual hypersensitivity.
Such drugs are relatively contraindicated for insulin-dependent diabetes mellitus and depression. If these pathologies are present, you need to weigh all the expected positive and negative effects before use.
List of drugs
Today the list of drugs is very large. Each drug listed below has a convincing evidence base and is actively used in clinical practice.
Non-selective drugs include:
- Labetalol.
- Dilevalol.
- Bopindolol.
- Propranolol.
- Obzidan.

Based on the above, we can draw conclusions about the success of using beta-blockers to control heart function. This group of drugs is not inferior in its properties and effects to other cardiological drugs. When a patient has a high risk of cardiovascular disorders in the presence of other concomitant pathologies, then in this case the role of beta-blockers is very significant.
When choosing a drug for treatment, preference should be given to more modern representatives of this class (presented in the article), since they allow for a stable reduction in blood pressure and correction of the underlying disease without worsening a person’s well-being.

