An acute infectious disease with a tendency to spread epidemic. Meningitis affects the soft lining of the brain and is almost always caused by a bacterial infection that begins in the ENT organs, including the sinuses, ears, and throat. A person of any age can get sick, but most often children under 5 years of age become targets for meningitis. Fortunately, thanks to antibiotics, purulent meningitis in developed countries is very rare today, whereas earlier whole epidemics of the disease broke out.
What is purulent meningitis
Purulent meningitis is a bacterial infection that causes inflammation of the soft membranes of the brain and spinal cord with the release of purulent exudate. It can develop as an independent disease or be a complication of an existing infection in any part of the body. Bacterial meningitis poses the greatest threat to life in comparison with other varieties of this disease (viral, fungal, or protozoal). Meningococcus and Haemophilus influenzae are called the leaders among the causative agents of bacterial meningitis.
Meningitis is an infectious inflammation of the soft membranes of the brain and spinal cordAs a contagious disease, meningitis spreads between people by airborne droplets or by contact. However, most people infected with meningococcus do not develop any clinical signs of the disease. About one in ten have symptoms of rhinovirus infection. Only in some cases, the pathogen spreads through the body through the bloodstream and a generalized form of infection develops. According to medical statistics, in developed countries, one of several tens of thousands of carriers of the infection falls ill with a generalized form.
The reasons for the development of the disease
Bacterial infections of the lining of the brain are caused by:
- meningococci;
- hemophilic stick;
- group B and D streptococci;
- pneumococci;
- staphylococci;
- salmonella;
- Pseudomonas aeruginosa;
- Klebsiella.
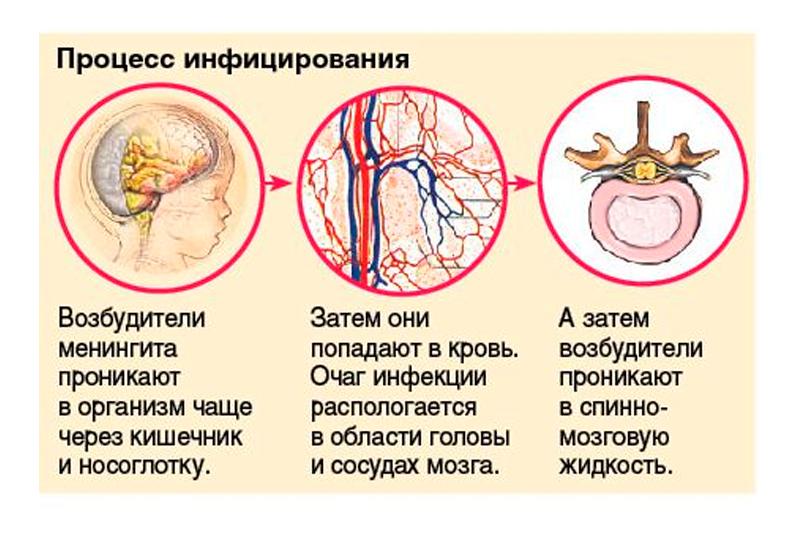 The causative agents of bacterial meningitis enter the body mainly through the nasopharynx
The causative agents of bacterial meningitis enter the body mainly through the nasopharynx Infection often occurs from a carrier or a patient with meningitis, but the pathogen can also invade directly into a wound during trauma or head surgery, including interventions on the paranasal sinuses. The penetration of a pathogenic microorganism into the blood and nerve tissues is facilitated by such factors as:
- recently transferred viral infections;
- a sudden change in natural conditions;
- previous traumatic brain injury or surgery;
- state of immunodeficiency.
The disease begins with the spread of the infection through the bloodstream. The bacteria then die and release toxins. After a short time, not only pathogenic microorganisms are found in the patient's blood, but also many toxic substances, which plays an important role in the development of the disease.
Meningococcal meningitis is a combination of generalized septic and toxic processes, as well as a subsequent allergic reaction.
During the progression of the disease, accumulated toxins affect small vessels: capillaries, arterioles, venules. The general vascular tone is impaired. As a result of damage to the microvasculature, there are disturbances in the functioning of vital organs, such as the brain, liver, kidneys and adrenal glands.
Disease classification
Depending on how exactly the pathogen penetrated the membranes of the brain, neurologists isolate bacterial meningitis: primary and secondary. The mechanism of development of the primary pathological process is triggered when the pathogen enters the nasopharynx cavity, where it was transmitted from the carrier into the bloodstream.
The reason for the development of the secondary form is a pre-existing focus of infection in the patient's body. The pathogen can enter the meninges through the blood or lymphatic bed from any place of chronic inflammation in the body, but most often such a focus is prolonged infectious inflammation of the middle ear or paranasal sinuses.
The severity of the pathological process determines one of three forms of the disease: mild, moderate or severe. The latter develops with severe immunodeficiency or in patients with an absent spleen.
The typical course of bacterial meningitis is acute.
Depending on the characteristics of the course of the disease, meningitis is:
- acute - rapidly increasing inflammation;
- lightning fast - characterized by an ultra-rapid progression of symptoms within a few hours;
- abortive - differs in a blurred clinical picture with a predominance of symptoms of intoxication;
- chronically relapsing - develops again after treatment.
Bacterial meningitis symptoms
The average duration of the incubation period of the disease does not exceed 5 days. Bacterial meningitis is characterized by an acute onset with intense, aggravated in an upright position and does not disappear after sleep. The condition is accompanied by fever (the patient's body temperature reaches 40 ° C) and symptoms of intoxication in the form of nausea and repeated vomiting. Disorders of consciousness are observed (adequate perception of reality suffers), mental overexcitation, signs of delirium. Convulsions are not excluded. Specific symptoms include stiffness in the muscles of the back of the head and neck. The intensity of symptoms increases from the first hours and worsens by the 2nd or 3rd day. Typical for patients is hypersensitivity to external stimuli: light, noise, wind. The appearance of hemorrhages on the body in the form of rashes or spots is possible.
Most carriers of meningococcus never develop the disease. But such people are capable of infecting others with an infection.
 Meningitis symptoms develop rapidly within 2-5 days after exposure
Meningitis symptoms develop rapidly within 2-5 days after exposure Purulent meningitis is accompanied by focal symptoms due to impaired transmission of nerve impulses in different areas of the skull. Pathology can affect the oculomotor nerves, which leads to limited mobility of the eyeball, visual split, ptosis of the upper eyelid. Less commonly, nerve damage develops:
- visual (the patient sees worse, suffers from loss of visual fields);
- vestibular cochlear (hearing loss develops);
- facial and trigeminal nerve (part of the face is immobilized).
 Hemorrhagic rash - small local hemorrhages caused by damage to the vessel by meningococcal toxins
Hemorrhagic rash - small local hemorrhages caused by damage to the vessel by meningococcal toxins When the inflammatory process covers the cerebral substance of the brain, this indicates the onset of meningoencephalitis. The focal symptoms characteristic of encephalitis are added to the manifestations of meningitis. This is partial or complete paralysis, speech disorders, loss of sensitivity, the occurrence of abnormal reflexes, excessive muscle tone. The patient has involuntary movements, hallucinations, impaired gait and coordination, memory disorders, sleep and wakefulness. Involvement in the purulent process of the ventricles of the brain is accompanied by attacks of excessive muscle tone in the limbs, limitation of flexion and extension movements of the legs and arms.
Manifestations of the disease in children
In young children, the disease has a clinical picture similar to adults, but in some cases it is expressed mainly by symptoms of intoxication, such as lethargy, loss of appetite, decreased overall activity, repeated vomiting. The threshold of sensitivity is increased, when the usual touch causes pain. Symptoms may be subtle in infants and are often confused at first with teething or other harmless conditions. The child becomes drowsy and lethargic, crying non-stop. Taking a closer look, you can notice other growing symptoms of a serious condition - trembling in the hands, pulsation of the fontanel, the manifestation of the venous network on the head and eyelids of the baby. Often, the skin becomes covered with red spots that form from hemorrhages as a result of multiple ruptures of the capillaries. Subsequently, the child may fall into a subcoma - a condition preceding a coma.
Diagnostics
A neurologist is involved in the diagnosis and treatment of the disease. A specific clinic, positive meningeal symptoms and signs of cranial nerve damage - all this allows the doctor to make a preliminary diagnosis. Diagnostics of the abortive form and secondary purulent meningitis can be difficult. In this case, the lumbar puncture will help to finally establish the causative agent of the disease - a lumbar puncture with a special long needle in order to collect cerebrospinal fluid for further analysis. In the pathologically opaque cerebrospinal fluid, a high content of neutrophils and protein is found. Bacterial inoculation of the material and its microscopic analysis make it possible to identify the pathogen.
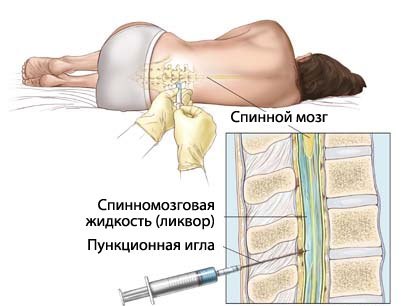 Lumbar puncture - collection of cerebrospinal fluid for further microscopic bacterial examination
Lumbar puncture - collection of cerebrospinal fluid for further microscopic bacterial examination Other necessary tests include a clinical analysis of blood and exudate secreted by elements of a hemorrhagic rash. Consultation of a narrow specialist (ENT, pulmonologist) may be required due to suspicions of a secondary nature of the infectious process.
Bacterial meningitis needs to be differentiated from intracranial hemorrhage, viral meningitis, manifestations of meningism in case of infection of the chest organs or inflammation of the upper respiratory tract.
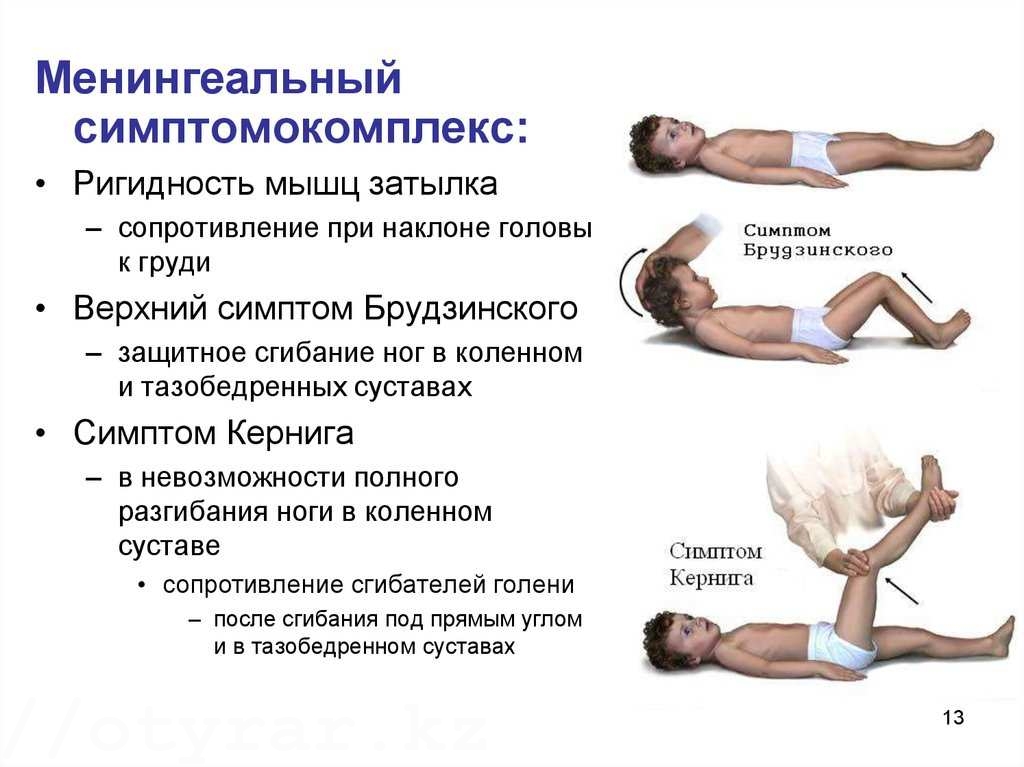 Meningeal syndrome is a symptom complex characteristic of lesions of the cerebral membranes
Meningeal syndrome is a symptom complex characteristic of lesions of the cerebral membranes The most specific meningeal symptoms are:
- the patient is unable to straighten the leg at the knee if it is bent at the hip joint;
- when the doctor tries to tilt the patient's head to the chest in a horizontal position on the back, his legs reflexively bend at the knees and hip joints;
- when trying to passively bend the patient's leg at the knee and hip, the other leg involuntarily takes a similar position.
Treatment
Bacterial meningitis of any etiology requires immediate hospitalization. Early diagnosis and treatment will prevent brain damage and death. Purulent meningitis is treated with intravenous antibiotics.
Drug therapy
An antibacterial drug is selected based on the origin of meningitis and its causative agent in each case. A combination of Penicillin or another antibiotic of the penicillin series is often used, for example, Ampicillin with drugs of the cephalosporin group (Ceftriaxone, Ceftazidime, Cefotaxime). Penicillins, like cephalosporins, are beta-lactam antibiotics that have a bactericidal (destroying microbes) effect. These drugs tend to disrupt the synthesis of the bacterial cell wall. The group of penicillins includes natural antibiotics and some semi-synthetic ones. But the main advantage of penicillins is low toxicity. They can be used in children and pregnant women.
With an unknown origin of purulent meningitis, empirical prescription of antibiotic therapy is possible. While the test results are pending, aminoglycoside preparations (Gentamicin, Kanamycin) are used, sometimes combining these drugs with penicillins.
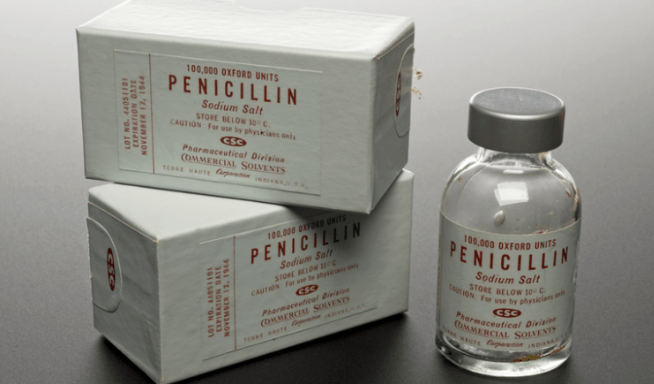 Antibiotics of the penicillin group are traditionally used in the treatment of meningitis
Antibiotics of the penicillin group are traditionally used in the treatment of meningitis To reduce edema and dropsy of the brain due to excessive accumulation of fluid in the ventricles of the brain, diuretics (Mannitol, Furosemide) are used. Glucocorticoids (Prednisolone, Dexamethasone) are prescribed to relieve inflammatory reactions. Symptoms are controlled with appropriate medications, which include:
- tranquilizers - drugs that have a sedative, hypnotic and anticonvulsant effect;
- lytic mixtures (for example: Diphenhydramine + Trimeperidin + Chlorpromazine) - a potent mixture of three medicinal components for the quick relief of seizures and psychomotor overexcitation, reducing fever and pain relief.
With a decrease in the volume of circulating blood and signs of septic shock, a blood transfusion is performed. Treatment of secondary purulent meningitis includes debridement of the primary infectious focus.
After the end of the acute stage of inflammation, the administration of neuroprotectors is shown, which prevent the development of destructive processes (death of nerve cells) in the brain, the treatment ends with a course of fortifying agents and vitamins.
Surgery
Secondary purulent meningitis caused by an ear infection is an indication for surgery to evacuate pus from the mastoid (the raised portion of the skull behind the ear). Modern powerful antibiotics in the vast majority of cases avoid surgery. But in the case of ineffectiveness of drug treatment or in the transition of the inflammatory process to the chronic stage, mastoidectomy is indicated. The intervention is performed under general anesthesia through an arcuate incision behind the auricle. Next, the skin and periosteum are gently shifted, then the underlying bone is trepanned (drilled) with a special medical chisel. Then the cells of the mastoid process are opened and the pus is drained, the affected tissues are removed. The wound is sutured, after placing a drainage tube in it to drain pus. Apply an antiseptic bandage. After the operation, the patient takes a course of antibiotic therapy.
Prognosis and consequences of purulent meningitis
Untreated bacterial meningitis is almost always fatal. With treatment, the risk of death is drastically reduced. So, the probability of death in newborns, provided adequate treatment is from 20 to 30%, in older children - about 2%. The likelihood of death is higher in adults, even with treatment, it ranges from 19 to 37%. Many adults who have had purulent meningitis may develop complications such as deafness (14%) or memory loss (10%).
The negative effects of bacterial meningitis are common. They can be temporary or permanent, occur immediately after an illness or in the long term. Adults who have undergone bacterial meningitis are prone to complications such as:
- septicemia, or blood poisoning - develops in 25% of those who have had meningococcal meningitis;
- hearing loss - may be partial or complete, therefore recovering patients need a hearing test;
- problems with memory and concentration;
- problems with coordination and balance;
- impairment of speech and vision (loss of vision can be partial or complete);
- mental illness and disorders such as depression, anxiety, increased fatigue.
Septicemia can cause gangrene. The abundance of toxins in the blood leads to the death of healthy tissue, especially the fingers and toes, or the entire limb. As a result, the limb can be amputated.
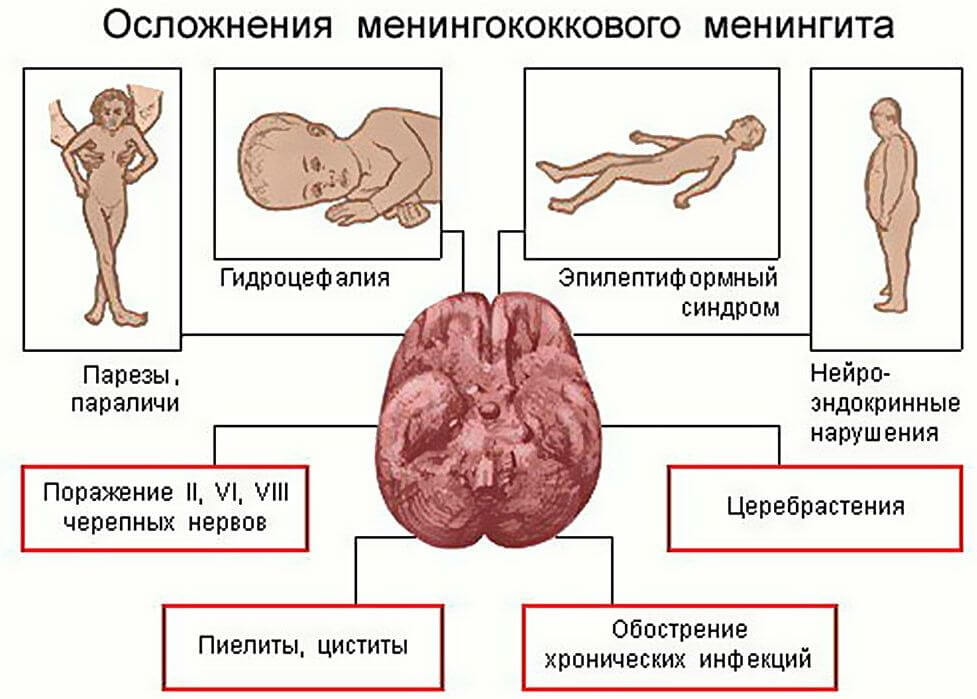 Purulent meningitis is dangerous for the development of formidable complications
Purulent meningitis is dangerous for the development of formidable complications Newborns who have had meningitis are at risk of developing cerebral palsy. This leads to a number of symptoms that affect movement and coordination. Many children have an increased risk of developing epilepsy after meningitis.
Children who have been ill can change their behavior, for example, become moody, irritable or even aggressive. Other complications of purulent meningitis in childhood include:
- sleep disturbances, nightmares;
- bed-wetting;
- psychological depression and fear of doctors and hospitals.
In general, children may have behavioral and learning problems after an episode of meningitis.
Prevention of purulent meningitis
Prevention consists in observing the basic rules of a healthy lifestyle:
- reasonable alternation of work / rest, adequate night sleep (at least 7-8 hours);
- to give up smoking;
- prevention of contact with sick people.
If contact with a person with bacterial meningitis cannot be avoided, then you should notify your doctor as soon as possible. He will prescribe a course of antibiotics for prophylactic purposes, which will significantly reduce the chances of developing the disease.
Vaccination is an important prevention tool. Bacterial meningitis can be prevented by vaccine medications such as:

Some types of meningitis are spread through close contact with an infected person's body fluids, such as saliva or nasal discharge. Avoid sharing drinks, utensils, and personal items that may contain saliva or other fluids from the patient. The steps outlined above will help prevent infection in most cases.
Purulent meningitis: video
Bacterial purulent meningitis poses a threat to the patient's life and requires urgent treatment. Timely adequate treatment increases the patient's chances of recovery and reduces the risk of serious consequences in the future.

