The brain is protected from external (mechanical) factors better than any other organ. In addition to the bones of the skull, it is protected from damage by the meninges. The fluid that washes the brain also acts as a shock absorber. However, traumatic brain injury (TBI) is one of the most common reasons for seeking help in medical institutions. In the general structure of injuries, TBI accounts for over 50% of cases, and in recent years there has been a tendency to an increase in their number, as well as to an increase in the severity of the injuries themselves. Last but not least, this is due to an increase in the pace of life (especially in cities) and an increase in the number of vehicles on the roads. Treatment of traumatic brain injury is the task of traumatologists and neurosurgeons. In some cases, patients require the help of neurologists and even psychiatrists.
Table of contents:Consequences of traumatic brain injury
A victim against the background of a head injury may have:
- mechanical violation of the integrity of brain tissue;
- violation of the dynamics of the cerebrospinal fluid;
- hemodynamic disorders;
- disorders of neurodynamics;
- the formation of scars and adhesions.
With concussions, reactive and compensatory changes develop at the level of synapses, neurons and cells.
Contusions are characterized by visible lesions and hematomas.
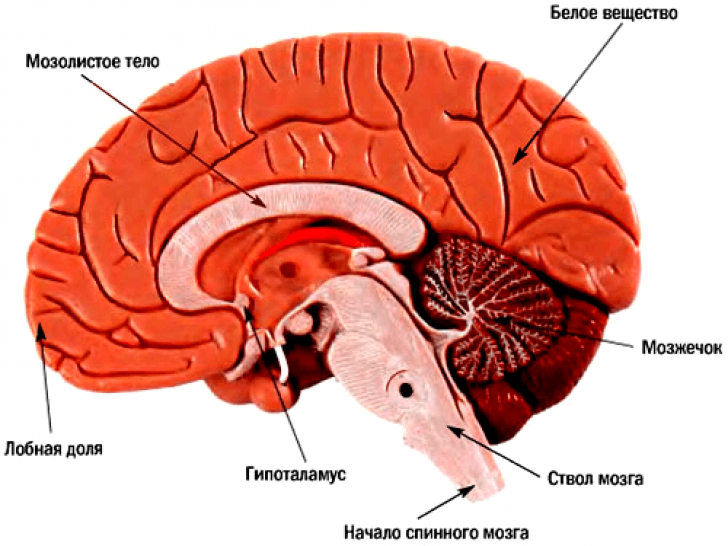
If in traumatic brain injury there is damage to the stem structures or the hypothalamic-pituitary system, a specific stress response develops, due to a violation of the exchange of neurotransmitters.
The cerebral circulatory system is especially sensitive to traumatic injuries. With TBI, a spasm or expansion of regional vessels occurs, and the permeability of their walls increases. A direct consequence of vascular disorders are disorders of cerebrospinal fluid dynamics.
Against the background of TBI, dysmetabolic disorders and hypoxia develop... Severe injuries can provoke respiratory and hemodynamic disturbances.
The so-called "traumatic illness" includes 3 periods:
- spicy;
- intermediate;
- remote.
Depending on the severity and type of TBI, the duration of the first period is from 2 weeks to 2.5 months. Acute phase is determined by a combination of a damaging factor and defense reactions. This is the time interval from the onset of exposure to a traumatic factor to the restoration of body functions or death.
V intermediate period the processes of lysis and repair in the damaged areas are active. At this stage, compensatory and adaptive mechanisms are turned on, contributing to the return of the impaired functions to normal indicators (or stable compensation). The duration of the second period can be from 6 months to 1 year.
Final (remote) period characterized by the completion of degeneration and recovery. In some cases, they continue to coexist. The duration of the phase against the background of clinical recovery is 2-3 years, and with the further development of the process, it is very uncertain.
Classification of traumatic brain injury
Note:injuries in this category are divided into closed, open and penetrating.

Closed TBI- These are head injuries, accompanied by the development of clinical symptoms, but without serious damage to the skin.
Open- these are injuries with damage to the layers of the skin and the aponeurosis of the skull.
Penetrating trauma differ in violation of the integrity of the hard shell.
Condition assessment
During the initial examination and examination of a patient in a medical facility, the following factors are necessarily taken into account:

The severity of traumatic brain injury is assessed by 3 factors:
- state of consciousness;
- vital functions;
- neurological symptoms.
Severity of TBI
- Satisfactory the patient's condition is considered if he has a clear consciousness, there are no violations of the most important functions, there are no primary and secondary neurological clinical signs. With timely and correctly carried out therapeutic measures, nothing threatens life, and working capacity is fully restored.
- For moderate injuries consciousness is clear or some stunning is present. Vital functions are not affected, but a decrease in the number of heartbeats is possible. Individual focal signs can be diagnosed. There is practically no threat to life with the timely provision of qualified assistance. The prognosis for full recovery from such a traumatic brain injury is quite favorable.
- In serious condition the patient has pronounced stunning or develops stupor - depression of consciousness, in which there is a loss of voluntary activity and reflexive activity persists. Respiratory and circulatory dysfunctions are recorded, and neurological symptoms are present. Paresis, paralysis, etc. are possible. The threat to life is quite obvious, and the degree of danger is determined by the duration of the acute phase. The prospects for full recovery after severe TBI are rather dubious.
- Signs very serious condition are coma, suppression of a number of important functions and pronounced neurological symptoms (both primary and secondary). The threat to life is very serious, and complete recovery from injury usually does not occur.
- The most dangerous condition is terminal ... It is characterized by coma, critical disorders of vital functions, as well as deep stem and cerebral disorders. Unfortunately, it is extremely rare to save the victim in such a situation.
Traumatic brain injury symptoms
Clinical symptoms allow us to draw preliminary conclusions about the nature of traumatic brain injury.
Concussion is accompanied by reversible cerebral disorders.
Typical symptoms:
- short blackout or (up to several minutes);
- slight stunnedness;
- some difficulties with orientation in space;
- loss of time from memory after injury;
- motor excitement (rare);
- (cephalalgia);
- (not always);
- decreased muscle tone;
- nystagmus (involuntary vibrations of the eyes).
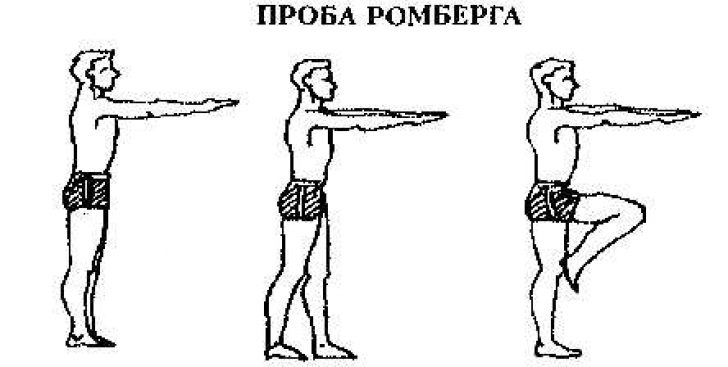
Imbalance in the Romberg position may be noted during neurologic examination. Symptoms tend to quickly regress. Organic signs disappear without a trace in the next 3 days, but vegetative disorders persist much longer. The patient may complain of vascular symptoms - a decrease or increase in blood pressure, cold snap and blue fingers, as well.
Bruises (UGM)
Clinically, there are 3 degrees of UGM - mild, moderate and severe.
Signs of a mild brain injury:
- loss of consciousness (up to 20-40 minutes);
- vomit;
- amnesia;
- cardiopalmus;
- (may be absent).
Moderate neurological symptoms regress by the end of 2-3 weeks after such a traumatic brain injury.
Note:the fundamental difference between a bruise and a concussion is the possibility of fracture of the bones of the arch and the presence of subarachnoid hematomas.
Signs of UGM of medium degree:

Neurological examination reveals meningeal and stem symptoms. The main organic manifestations subside in 2-5 weeks, but some clinical signs of a previous traumatic brain injury make themselves felt for a long time.
Signs of severe UGM:
- consciousness is absent for up to several weeks;
- there are life-threatening violations of essential functions;
- motor excitement;
- paralysis;
- hypo- or hypertonicity of the muscles;
- convulsions.
The reverse development of symptoms proceeds slowly, there are often residual disorders, including from the side of the psyche.
Important:a sign that with 100% probability indicates a fracture of the base of the skull is the release of cerebrospinal fluid from the ear or nose.
The appearance of symmetrical hematomas around the eyes ("glasses") gives grounds to suspect a fracture in the area of the anterior cranial fossa.
Compression
Compression often accompanies bruises. The most common causes are hematomas of various localization and damage to the bones of the arch with their depression. Less commonly, damage is caused by swelling of the brain tissue and pneumocephalus.
Symptoms of compression can sharply increase immediately after a traumatic brain injury or after a certain ("light") time interval.
Typical signs of compression:
- progressive impairment of consciousness;
- cerebral disorders;
- focal and stem signs.
Probable complications of TBI
The greatest danger in the acute phase is represented by dysfunctions of the respiratory system (respiratory depression and disturbance of gas exchange), as well as problems with the central and regional (cerebral) circulation.
Hemorrhagic complications are cerebral infarctions and intracranial hemorrhages.
In severe craniocerebral trauma, dislocation (displacement) of the parts of the brain is possible.
Against the background of TBI, the likelihood of complications of a purulent-inflammatory nature is quite high. They are divided into intracranial and extracranial. The first group includes abscesses, and, and the second, for example,.
Note:probable complications include post-traumatic and.
First aid for traumatic brain injury
 Important:first aid for traumatic brain injury is to provide the victim with complete rest. He needs to be given a horizontal position with his head elevated. If the patient is unconscious, it is impossible to move him, since the likelihood of a spinal injury cannot be ruled out. It is advisable to apply a heating pad with cold water or an ice pack to the head. If breathing or cardiac activity stops, before the arrival of the ambulance, resuscitation should be carried out - chest compressions and artificial respiration.
Important:first aid for traumatic brain injury is to provide the victim with complete rest. He needs to be given a horizontal position with his head elevated. If the patient is unconscious, it is impossible to move him, since the likelihood of a spinal injury cannot be ruled out. It is advisable to apply a heating pad with cold water or an ice pack to the head. If breathing or cardiac activity stops, before the arrival of the ambulance, resuscitation should be carried out - chest compressions and artificial respiration.
Primary care for patients is provided at the nearest medical facility. The volume of primary care is determined by the severity of the patient's condition and the capabilities of physicians. The primary task of doctors is to maintain respiratory and circulatory functions. It is imperative to restore airway patency (this is often impaired by aspiration of blood, secretions, or vomit).
Treatment of any craniocerebral trauma is carried out in stationary conditions... Depending on the nature and severity of the damage, they resort to conservative tactics or perform neurosurgical intervention.
With psychomotor agitation or convulsions, relaxants (for example, Diazepam) are administered intravenously. Symptoms of constriction are a good reason for prescribing a diuretic. If there is a threat of edema, osmodiuretics are used, and the victim is immediately delivered to the neurosurgical department.
 To stabilize blood circulation, vasoactive pharmacological agents are administered, and if there is a likelihood of hemorrhage in the subarachnoid space, hemostatics are indicated.
To stabilize blood circulation, vasoactive pharmacological agents are administered, and if there is a likelihood of hemorrhage in the subarachnoid space, hemostatics are indicated.
In the treatment of traumatic brain injury, neuroprotectors, neurometabolic stimulants, vitamins and glutamic acid are widely used. To combat CSF dynamics disorders, dehydration drugs are needed.
The duration of treatment depends on the type and severity of TBI and the dynamics of the recovery process. Even with mild concussions, the patient is shown to stay on bed rest for one and a half weeks.
Plisov Vladimir, medical columnist
147 voices, medium: 4,56 out of 5)
