Pain in the field of the back, especially in the lower part, one of the most frequent reasons Appeals to neurologists. The most common diagnosis is osteochondrosis, which includes the morphological change in the bodies of adjacent vertebrae and degenerative change Intervertebral disk, called hernia. The hernia is just a degree of dystrophic change of intervertebral cartilage, its thinning, loss of elasticity, replacement of hyaline fibers with fibrous.
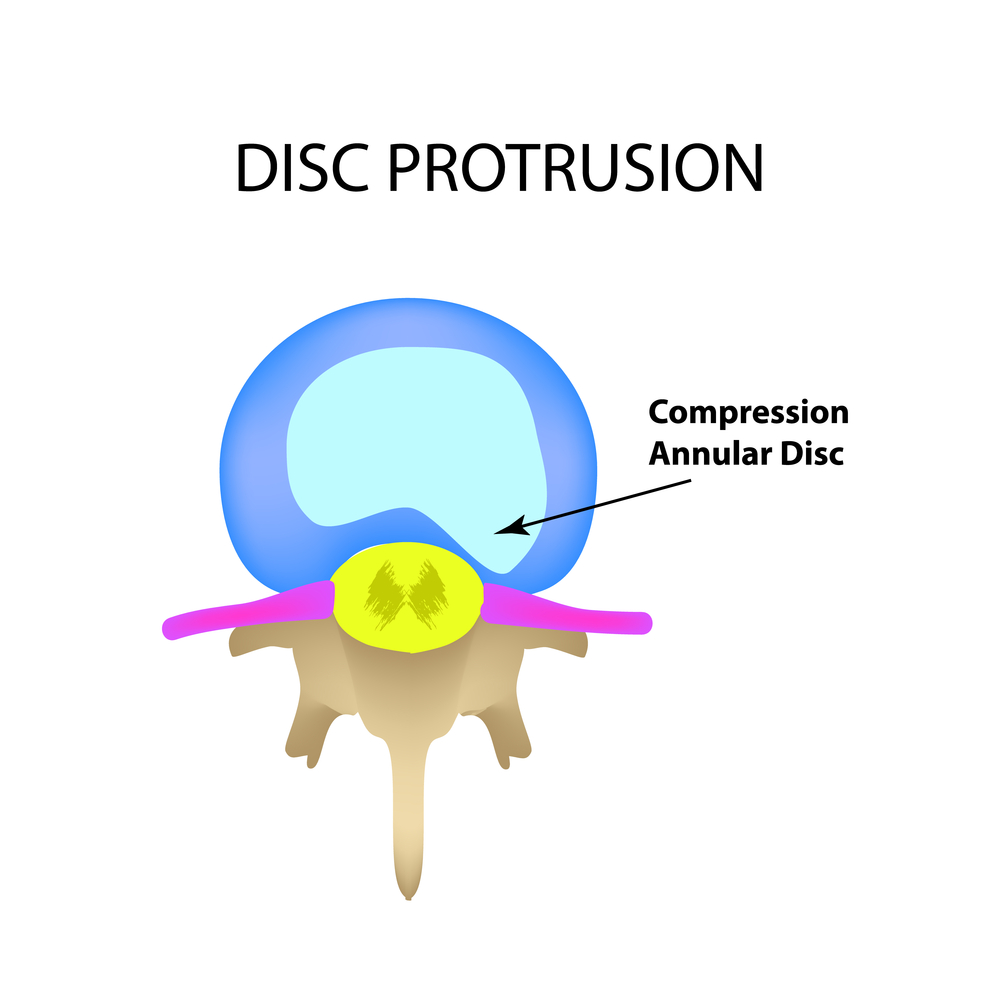
What is hernia intervertebral disc? The intervertebral disc is an articulation between two vertebrae. It consists of a student student of the central core and is surrounded by a concentric ring ring of cartilage. When there is a degeneration disk, cracks appear in the ring space and allow you to migrate the part of the kernel outward, forming a projection that squeezes the adjacent nervous root, this is a disk hernia.
Often very painful, the hernia of the intervertebral disc affects mostly people aged 25 to 55 years old, mostly men. This can happen anywhere in the spine, but most often it occurs in the neck and lower back area. This is the second leading cause of the disease of the disk.
The structure of the intervertebral disc
The intervertebral disc is a gasket of a rounded form between two adjacent vertebrae. This disk carries a support and amortization function, provides a certain mobility. spinal column. Outer side The disk is a fibrous ring consisting of intersection of collagen fibers.
What are the symptoms of an intervertebral disk hernia? First of all, note that the hernia of the intervertebral disk may be asymptomatic, i.e. She does not manifest any symptom. In addition, its manifestations can vary greatly from one subject to another.
Most of the time we are talking about a strong and strong pain in the area, affected by the hernia of the intervertebral disc. The hernia of the intervertebral disc is the bloating of the part of the intervertebral disk, in particular, the jetty kernel. This protrusion can then squeeze the neighboring nervous structures, such as the spinal cord and the roots of the spinal nerve.
Inside the fibrous ring is a journalist (pulpous) core consisting of cartilage cells, not large number Collagen fibers and a large amount of an intercellular substance that can hold moisture inside the kernel to provide a turgora. Numerous clinical studies have shown that there is a permanent and active exchange of liquid media between the kernel of the disk and tissues surrounding it.
Causes pain in the lower back, often one-sided. Which radiates into the buttock and low limb. The pain is enhanced when the back muscles are bent during sneezing, tensions and long stay, sitting or lying on the stomach. Sometimes neurological deficiencies sometimes seem sensory: tingling, numbness, tingling, sometimes the motor: weak muscleswhich can reach the paralysis. In more heavy casesWhen the spinal cord affects, the anal and urinary sphincter disorders can be noted, and then - emergency medical care.
The role of the intervertebral disc and its participation in the cases of the hernia disk. The case of the disk hernia involves a local joint unit. Intervertebral discs are flexible discs comparable to shock-absorbing pillows, which are located between 24 vertebrae of the spine. These specialized joints have the function of vertebrae permission to move, soften the forces that compress them and stabilize the vertebra. The mobility of the vertebral makes it possible to power and regenerate the articular tissues, steady mechanical stress or injury may threaten the balance between normal wear and regeneration, which is the guarantor of the integrity of the articular tissues. This movement loss leads to degeneration of joints; Consequently, vertebral dysfunction.
Types and types of dystrophic changes of the intervertebral disk
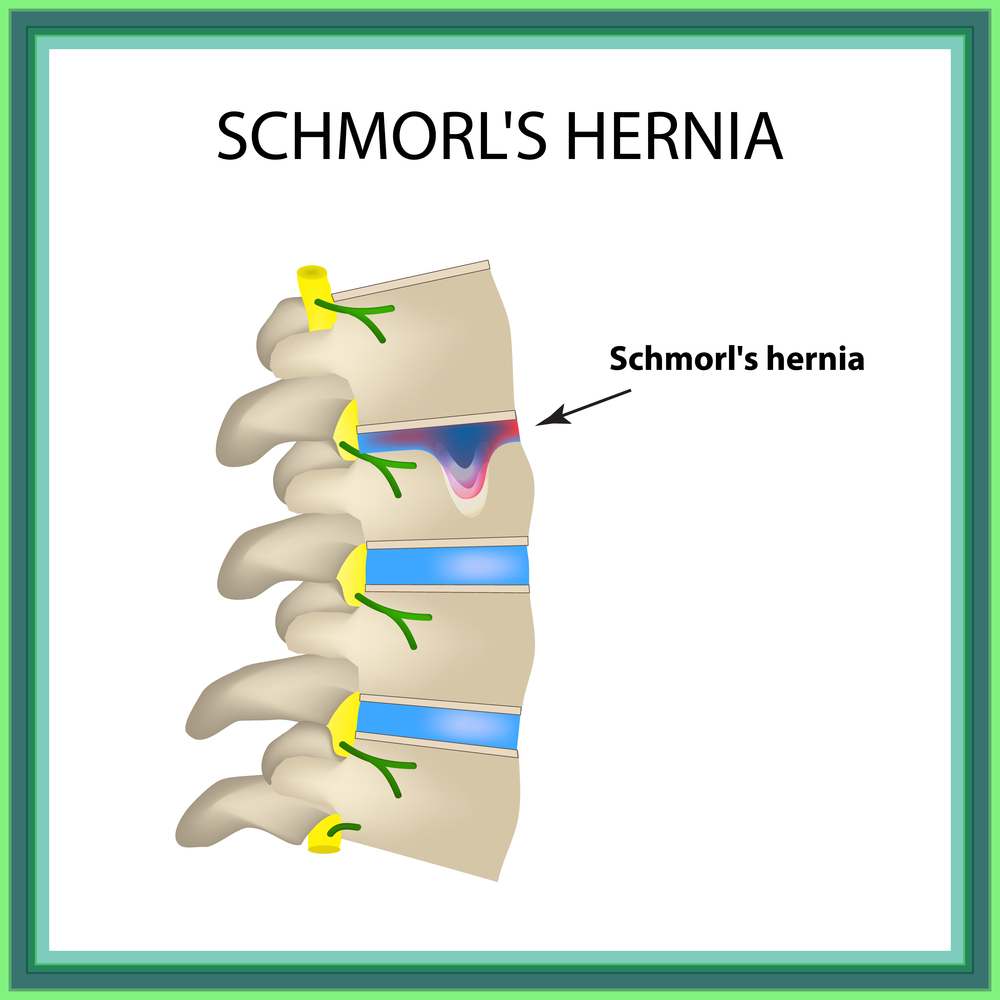
The hernia of the disk is a pathology, in which parts of the damaged and modified pulp nucleus are squeezed through the defect of the fibrous ring, provoking its gap or excessive protrusion for normal physiological boundaries, fall into the cavity of the spine canal or "pressed" into the body of the vertebra. If the fibrous ring is saved, its protrusion under the action of the sequestles of the altered coder is designated as a protrusion (protrusion) of the disk. Often the term "prudrusion" is used to indicate the size of the hernia, which leads to an incorrect interpretation of the state.
The intervertebral disk consists of two elements: a centered central kernel and fibrous rings that surround it and save it. These fibrous rings allow the dismissal of deformation and prevent any core offset. In the case of constant compression, cracks may occur in fibrous rings, which will create a gap through which the kernel will go out and act. This will create compression or irritation of nervous roots located nearby.
This problem may be the result, among other things, overwork, sudden grinding of the trunk or lifting heavy loads. Pregnant women, high people And people with overweight are especially exposed to risk. During the first consultation on chiropractic, the manual therapist will perform the history of the disease, the patient is proposed to describe the pain he experiences, the frequency, the intensity of these and their location. Then he will follow the inspection of chiropractors to learn more about the pain of the patient. When indicated, it will take x-rays spine.
It should be borne in mind that there is a physiological discharge of a disc that occurs under the action of the axial load and, as a rule, not exceeding 3 mm. If the protrusion is common, leads to a narrowing of the spine channel and does not change its size when the spine is moved - it is a pathological protrusion. The absorption of the intervertebral disc is considered to be clinically significant if it exceeds a quarter of the diameter of the vertebral channel or narrows the channel to a critical level of 10 mm.
This information will allow chiropractic to establish the correct diagnosis and the appropriate care plan. In many areas, we use the proverb "Prevention is better than treatment", and it also applies to hernia intervertebral disks. Indeed, it is always better to save your back to prevent small problems that may worsen later.
So avoid physical actionwhich can be subjected to stable mechanical stress, injury and / or all that can be a source of permanent compression on intervertebral discs. In addition, you can follow a few simple recommendationsTo save your back and your discs, for example.
Thus, the diagnosis of the "disk hernia" denotes the case of penetration of the pulp nucleus through the gap of the fibrous ring beyond its limits or into the body of the vertebral, proceeding the guial plate (that is, the perforation of the plate arises).
In the direction of the loss of the sequestrate, hernias are distinguished:
- Advanced: They will try forward longitudinal bonds, motor and sensitive disorders do not cause. Could provoke sympathegical syndrome when involving a sympathetic paravertebral chain in the process.
- Purples: It is they who pose a threat to the contents of the spinal canal and cause serious neurological disorders.
In relation to the median line allocate:
Keep your back straight, without twisting the trunk when lifting the cargo, carrying next to the body.
- Do not stop for a long time, especially when sitting.
- Choose office furniture that can be adjusted in height and slope.
Manual therapy is aimed at restoring mobility of vertebrates so that the body can cure himself. In combination with rest for several days, this help gives unexpected and long-term results. It is obvious that the exercises are necessary to strengthen and stabilize the spine and musculature of the pelvis.
- median hernias: often have big sizes, Sometimes they can penetrate into the subarachnoid space, while part of the sequestration can move along the length of the space. These hernias often squeeze the spinal cord in the cervical and chest departments, horse tail at the lumbar level, causing paresa and violations function pelvic organs. Often it is these hernias that determine the chronic pain process.
- paramedian hernia: are the cause of radicular syndromes with the damage to the roots spinal cord, especially at the level of the two lower lumbar drives.
- pure side hernias: located in intervertebral holes and lead to the infringement of the roots located there. Sometimes they can squeeze the front root artery, which can lead to a spinal cord heart attack.
- Herniation of the Schimor (hernia bodies of the vertebrae): more often appear in young age. Single forms of these hernia indicates osteochondrosis or injury. In most cases, they are asymptomatic and are a "radiographic find".
IN clinical practice Used gradation in the development stage of hernia:
Louis Philipp Maureen, Chiro in Quebec with 38-year-old experience, offers chiropractic in Chiropractic clinic in Sillery, Stey-Foy - Quebec. The difference between the hernia sharp disk and chronic disk hernia? All this is a matter of time. In the case of acute hernia of the intervertebral disc, in a few hours or days before that, the brain was normal, then the "destruction" of the disk kernel came across and was deformed from paralysis. This type of hernia is painful. In this case, the surgeon must quickly free it, but he can't do anything about internal damage bone marrow.
- Prolapping - protrusion of the intervertebral disk in size of 2-3 mm.
- Protrusion - disk protrusion from 4-5 mm to 15 mm without nuclear displacement beyond the fibrous ring.
- Extrusion - degeneratively modified kernel goes beyond the fibrous ring, often observed a disc fragment in the form of a drop.
- Sequestration - the loss of the substance of the student core in the spinal channel.
Most often there are croves of disks in the lumbar department (up to 80%), less frequently find changes in the breast spine (about 1%).
This is an image of a finger stuck in the door that the surgeon produces from the door, but the injuries of the crushing in the finger there is still there. The surgeon can reduce or even cancel deformation, but the brain will remain atrophied forever. Operated animal is in best conditions Anesthesia, asepsis and possible technicality. We especially want to fine with the pain that this operation can call in the first wake-up hours, so such a patient remains hospitalized at least 48-72 hours.
As a rule, the pain rises beyond, and the first signs of improvement are manifested either during hospitalization or in the first days of returning home. Unfortunately, the exception always confirms the rule, and sometimes it is necessary to be more patient or revised the operation of the surgeon using the new imaging stage. Rehabilitation is rarely necessary in most cases of acute hernia; It can be suggested during chronic hernia, because the spinal cord atrophy requires much slower recovery.
Causes of the appearance of intervertebral hernia
- Incorrect posture (scoliosis, kifoscolyosis), undeveloped muscular corset, pathological motor and positional stereotypes.
- Lifelong lifestyle, long stay in a monotonous posture, static loads.
- Power and contact sports, improper weight lifting.
- Injuries.
- Congenital abnormal development of bone, cartilage, connective tissue, spinal column.
- Age changes, osteoporosis.
The hernia disk is one of the most common diseases in Italy with very high social costs. In fact, about fifteen million Italians suffer from back pain more or less seriously and, according to statistics, this is the first cause of abssent effect from work and, depending on the constant invalidity. Unfortunately, unfortunately, it often met an extremely diverse diagnostic and therapeutic route, in the form of his Ping Ponga from orthopedic to a physiotherapist, to a neurologist.
All this is due to the fact that this wonderful structure, which is backpacked by a person, can represent many unwanted and curable discomforts from different points of view in accordance with the "kosk" or "sector". Very often, the traditional "back pain" is due to the presence of pathologies, such as the symptomatic hernia of the lumbar disc, which is a degenerative disorder of the intervertebral disk, and manifests itself with a clinical picture characterized by pain in the back, the radiculopathy of the compression of the Ishiaas or shoulder Sustav and restrictions or functional impotence.
Symptoms of intervertebral shelter
All symptoms can be divided into 2 groups: irritation and lesions.
When irritating the spinal cord and nerve roots develop pain syndrome Various degrees of intensity, local or irradiating along the irritated root. Often there are violations of sensitivity in the form of paresthesies, feelings of numbness in the limbs. At the same time, deep and vibration sensitivity decreases, tendon reflexes can increase.
Lumbar pain from disk protrusion and root compression is a problem that has a special social value. Indeed, 55% of the population of Western countries reports at least, once in life, Episode of Lyumbahoatria and 80% simple spine. But the most common cause of Lubagagoathemia remains herniation of an intervertebral disc, whose natural history includes permission in 50% of cases clinical picture Because of its retention for 8-9 months after the start.
Excusable methods are in a particular case of efficiency comparable to the effectiveness of surgery, but with a smaller risk of relapses due to an external approach to the spinal channel and much less invasive, which reduces the hospitalization time, and also have the advantage to be repeated, not excluding, in case of failure , The use of traditional surgery. They allow you to optimally manage low-cost patients and minimal risk, which makes it possible to successfully cope with such a frequent disease.
For organic lesion Structures nervous system The symptoms of the fallout occur: a decrease in tactile and painful sensitivity up to anesthesia, atrophy and reduced strength and tone of muscles innervated by damaged root, violation of the function of pelvic organs, chronic pain syndrome. In neurological examination, there is a decrease or loss of tendon reflexes, the emergence of pathological engine signs.
Ozone also acts on the mucopolysaccharide component of the pulp kernel, causing depolymerization by the release of water molecules, leading to dehydration disk. Within a few weeks there will be a decrease in the volume of the disk, which will slow down the hernia with a decrease venous stagnation and the compression effect on the nervous root and, therefore, from pain. Comparison of the results with other percutaneous techniques is extremely satisfactory, in the face of risks and complications is not statistically significant.
Actually, allergic reactions reported as a percentage of patients equal to 0, 5%. The laser determines the evaporation of a small number of pulp kernel, but quite small to determine the sharp and noticeable decrease in the nerve pressure on the compressed and compressed nerve. The patient must observe 24 hours of absolute rest.
Diagnostic criteria
 For setting exact diagnosis The doctor first holds an objective examination, and then assigns additional diagnostic methods.
For setting exact diagnosis The doctor first holds an objective examination, and then assigns additional diagnostic methods. When painful syndrome appears in the back area, you must contact a doctor. In addition to pain caused by hernia, there is a mass of other etiological reasons that need to differentiate.
As part of our institution, a therapeutic diagnostic path for a discusar nerve, aimed and effective, allowing the patient to show appropriate symptoms for the patient a short timeto get proper diagnosis and appropriate treatment, avoiding long blocking it everyday life. Duration, often characterizing the path of diagnostics and, therefore, related to these therapy is associated with the lack of proper and comprehensive information on patients with the hernia of the lumbar disk or stenosis of the spine canal, provided about the benefits and risks surgical treatment.
For the setting right clinical diagnosis An inspection of a doctor is very important. The doctor must be very carefully referring to the complaints and anamnesis of the disease. It is necessary to clarify the localization and character of pain, in which position pain is enhanced, and in which it subsides, is there an irradiation of pain, there are motor and sensitive disorders, the time of day with a peak of pain. It is equally important to find out the beginning of the disease provoking factors, the dynamics of the development of symptoms. It is necessary to stop in detail on the lifestyle, working conditions. The following should be neurological examination with the study of reflexes, sensitivity, tone and muscle power, the presence of pathological motor signs, tension symptoms. After that, it follows a palpator inspection to identify disruption of the biomechanics of the spine, trigger points, the redistribution of the muscle tone. After conducting such a thorough inspection and detailing complaints and history, the doctor can put a preliminary diagnosis.
The next step will be x-ray. This method will not give an accurate answer about the presence of hernia, its size and location, because X-ray rays pass through hernia. But exist radiographic signswhich will indicate a possible affected segment. This method of research is rather screening, the cost of research is small, but the method allows you to determine which studies are necessary in the future, and at the early stage of diagnostics, other pathologies helps to differentiate.
In the same stage it will be advisable to hold clinical study Blood with revpets. This will help confirm or eliminate inflammatory or rheumatological diseases.
Computed tomography and magnetic resonance study allow the most accurate visualization of the presence of hernia, its relationship with the surrounding structures, the size of the protrusion, the state of the pulp nucleus. CT allows you to more clearly see dense bone structures, spinal cord he visualizes worse. But this method is cheaper, and it is more often used to study the lumbosacral spine. MRI preferably use when studying the cervical department and when the doctor suspects inclusion in pathological process spinal cord. This study is expensive, he has more contraindications.
Treatment of an intervertebral disk hernia
With initial manifestations of pain and neurological syndromes caused by the hernia disk, pharmacotherapy is used. Analgesics, steroid and nonsteroidal anti-inflammatory drugs, vitaminotherapy, chondroprotectors, muscle relaxants, anticonvulsants, drugs that improve blood circulation are used. Medical therapy It is good to combine with physiotherapeutic treatment. Methods such as the effects of diadynamic currents, magnetotherapy have proven positively. There are methods for introducing certain drugs to the area of \u200b\u200bdamage using electrophoresis.
With a decrease in the severity of pain syndrome, you can resort to help manual therapist, massage therapist. It is useful to use such techniques like a postisometric relaxation, underwater and dry stretching, exercises on the EMMNOVA board. And, of course, therapeutic physical culture for the formation of the correct posture and the muscular corset.
Do not forget about needleflexotherapy, pharmacopuncture.
There are methods of surgical treatment of hernia of intervertebral discs. Indications for such operations are very limited: increasing paresis, violation of the functions of pelvic organs, disabled with pain syndrome. Some doctors believe that the presence of sequest-end hernia is also an indication of surgical intervention. There are several ways operational treatment, choose the most suitable method For each patient individually.
Any of the methods of treatment implies a change in lifestyle, the formation of the correct stereotypes of physical and static activity, work on oneself. Without this, treatment will be ineffective and the disease may return.
TV channel "Russia-1", transmission "On the most important thing" on the topic "Intervertebral hernia".
Intervertebral hernia - serious diseasewhich is manifested not only by strong pains in the back, but also a violation of the function of the spine and failures in the work of the internal organs. So, with hernia in cervical department It is often manifested in long and regular pains in shoulders and arms, high fatigue.
The hernia of the intervertebral disc breast Department entails, in addition to pain in the spine itself, easy sensations in the heart and lungs. And with diseases of the lumbar department, legs suffer. If you do not fulfill timely and competent treatment intervertebral herrojithen there is a high probability of complete or partial paralysis.
According to statistics, the intervertebral hernia is diagnosed in 75% of all patients accessing a specialist with complaints of pain in the back, neck, lower back. Modern osteopathic techniques make it possible to effectively effectively diagnose and deal with this disease without operational intervention. Therefore, it is so important to contact a specialist at the first symptoms when it is possible to eliminate the hernia easy enough and quickly.
What is intervertebral hernia
The intervertebral disk is a "puck" from a fibrous fibrous tank, impregnated with liquid (water), which acts as an amorticing gasket between two vertebrae. Due to its porous elastic structure, the intervertebral disc is compressed under load, the release of the moisture contained inside and the prevention of the vertebra from contact and friction. When the spine is unloaded, the disk is rebounded by moisture from the surrounding tissues, taking the previous form.
With constant loads - for example, lifting weights - time to rehydrate the disk during the unloading of the spine is not enough. Often surrounding the fabric disk simply do not contain enough liquid, because of which the disk is deformed by shifting relative to the vertebrae.
After some time, constant deformation and displacement in combination with the load on the spine leads to the fact that the fibrous membrane of the disk is broken, and the kernel, softer and elastic, is partially outward through the gap.
Traditional medicine with intervertebral hernia
Treating hernia methods traditional medicine It is quite widespread and demonstrates good efficiency. Unfortunately, minus the traditional approach in the symptoms of such treatment. If we are talking about surgical interventionThe intervertebral "breakdown" hernia is not restored and is removed or evaporates with a laser, which leads to serious damage or complete destruction of the disk. Thus, the joints, between which the hernia was located, are articulated with a violation, and often with complete loss of mobility. That is, the symptoms of the disease are destroyed, the pain goes, but the spine itself is not restored. Osteopathic treatment in this regard is more gentle.
Causes of the formation of intervertebral hernia
Typically, the reasons for the formation of intervertebral hernia are prolonged physical exercise and age wear of the body. That is why the disease is most often manifested in age after 40 years. Moreover, the physical exertion themselves do not necessarily lead to intervertebral hernia, they only contribute to the deformation of the disk and its displacement.
Directly to the rupture can lead simply careless movements. In this case, part of the disk core, squeezed out through the gap, can contribute to pinching the nerve endings, which becomes the cause of regular strong painwho are not localized on the damaged area of \u200b\u200bthe spine, and distribute and "are given" to the head, arms, legs, internal organs.
To factors provoking the displacement and deformation of intervertebral discs and the subsequent development of intervertebral hernia include:
- Continuous long-term loads affecting the spine and squeezing discs.
- Long stay in a standing or sitting position. Especially dangerous last, because at the same time huge pressure Come on the spine.
- Sharp movements, turns that can lead to injury and disk displacement.
- Excess weightwhich is why the spine accounts for an increased load.
- Injuries of the back and spine when hitting.
Symptoms of an intervertebral disk hernia
The symptoms of intervertebral hernia are explicitly manifested as the disease develops. In the first stages it may be easy increased fatigue, fatigue, susceptibility to loads. Pain in the back, hands or legs manifest only after long-term physical exertion, at the end of the working day.
Over time, pain become more pronounced and can manifest themselves in careless movements, especially twisting. Also, pain feels are felt when lifting weights with flashed back.
The symptom indicating the sufficiently serious development of the disease and the need for urgent treatment of hernia are pain, "outstanding" to other parts of the body. This happens already on late stages Diseases when intervertebral hernia passes nervous roots.
Osteopathy in the treatment of the hernia of the intervertebral disk
Osteopathic techniques demonstrate high efficiency in the treatment of the hernia of the intervertebral disc, especially on early stagesWhen the fibrous disk is not yet happened yet. Therefore, it is so important to diagnose the disease as early as possible. Osteopath will also help it. A specialist can quickly find changes that lead to hernia.
With osteopathic treatment used a complex approachwhich lies not only in the use of manual technician, but also in correction of the power mode, dispensing of physical exertion, the appointment of exercise of the exercise of exercises and other physiotherapeutic procedures. Manual impact is aimed primarily for the relief pain sensations, without which further treatment It will be simply impossible. Impacting muscles and bones, joints and internal organs, osteopath achieves them as relaxing, removing various spasms and blocks that impede the normalization of the entire body in general.
As intervertebral discs Do not have its own blood supply system, their nutrition is liquid, useful substances and vitamins occurs through neighboring fabrics (mostly muscular). Involving the vitamins, the "construction" material and moisture in full leads to the fact that after the deformation, the disk does not restore its original state, which provokes the hernia.
The second stage of treatment at Osteopath is just to form proper nutrition Patient and provide tissue by all required substances. It is important that the surrounding tissues are fully supplied by them through blood system. To do this, in the treatment, various manual, massage and cranial techniques are used, which improve blood circulation not only on the pricing plot, but in the whole body.
The final stage of treatment of intervertebral hernia lies in the effects of the damaged vertebrae and wheels, which, with the help of manual techniques, a specialist puts in place. Usually, the treatment of hernia requires the application of the following techniques:
- stretching muscles and vertebrae;
- the kneading muscular corset;
- rhythmic effects to restore the body's macropulsia;
- inhibition;
- vibrational impacts carried out with varying degrees intensity;
- euphluory.
The features of the above techniques are that each of them individually and in combination is absolutely safe for the body. Therefore, they can be prescribed even at the first symptoms of intervertebral hernia with almost age-related restrictions.
LFC techniques ( medical physical education) are a mandatory component of comprehensive treatment. They allow the patient to learn how to move and keep the back in such a way as to eliminate disk offset regarding the vertebrae. In addition, moderate physical exertion (performed under the supervision of the doctor or independently) allow you to strengthen the muscular frame, make your back stronger and stable precisely at the expense of muscles, not bones.
For the period of treatment, as well as after its completion as preventive tool Different maintenance designs are used: belts, corsets with sufficient rigidity and retaining spine from incorrect position and displacement of intervertebral discs.
Although the intervertebral hernia is a serious illness, the treatment of which may require a lot of time and strength, can be completely healing the patient modern methods. Osteopathy works most effectively in a complex with other procedures and techniques. But you can only trust the treatment only by an experienced specialist who can pick up a power plan and assign the required complex. exercise. As practice shows, only with this complex treatment You can achieve high results and quick recovery.

