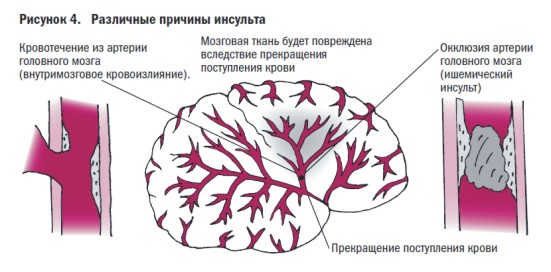
Ischemic stroke is an acute disorder of cerebral circulation in a certain arterial basin, which leads to a focus of necrosis of brain tissue and is accompanied by persistent neurological deficit that persists for more than 24 hours.
Ischemic stroke is the most common form of cerebrovascular accident and accounts for about 80%. In our country, the mortality rate from this disease remains one of the highest in the world; more than 400 thousand strokes are registered annually, which, if not fatal, lead to permanent disability.
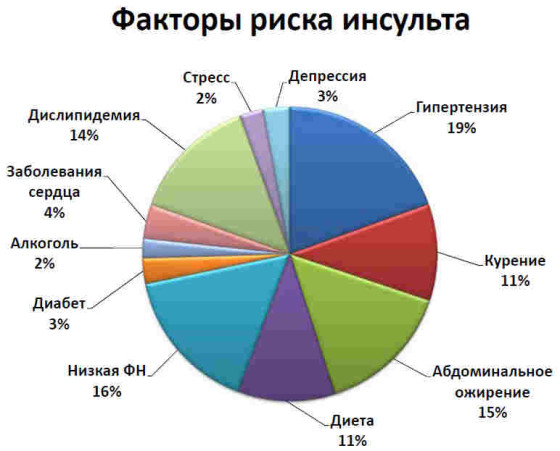
Risk factors for stroke
Forewarned means forearmed, therefore, if you know what causes this disease, can be prevented this disease. Risk factors for stroke include:
- atherosclerosis;
- hypertension (untreated hypertension with blood pressure values more than 200/100 mm Hg increases the risk of getting sick 10 times);
- IHD (especially the presence of rhythm disturbances such as atrial fibrillation);
- diabetes;
- smoking;
- obesity, hyperlipidemia;
- history of TIA;
- male gender (stroke occurs more often in men);
- elderly age.
I would like to note that at present stroke is not considered as a separate nosological unit, but for it a single etiological factor can be identified - atherosclerosis.
Symptoms of ischemic stroke

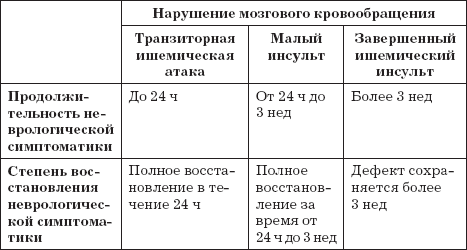
Depending on the degree of disturbance of cerebral blood flow, the following options for the manifestation of a stroke are possible:
- acute onset: quick appearance neurological symptoms and deficits, the patient can clearly indicate the time of onset of the disease. This course is typical for the embolic variant of stroke (the patient has atrial fibrillation);
- undulating onset: symptoms of the lesion are of a “flickering” nature, gradually increasing over time;
- tumor-like onset: ischemia increases over a long period of time, affecting the main vessels of the brain, which ultimately leads to a full-blown stroke with a large area of damage to brain tissue.
The first signs of a stroke that the patient should pay attention to:
- speech impairment or difficulty;
- pronounced headache, which does not go away after taking NSAIDs;
- weakness and numbness of the limbs, half of the body;
- severe dizziness, which is accompanied by nausea and vomiting;
- disturbance of orientation in space, time and self;
- sudden blindness in one eye or loss of visual fields.
Everyone needs to know the dangerous symptoms, since failure to seek treatment in a timely manner medical care significantly worsens the prognosis of the disease. The sooner a patient seeks specialized medical care, the greater the chance for a speedy recovery and restoration of lost functions, since time counts by minutes.
Stroke classification
The most common is the TOAST classification, which distinguishes the following options:
- cardioembolic: emboli are blood clots that form in the heart cavity during atrial fibrillation, mitral heart disease, or recent myocardial infarction;
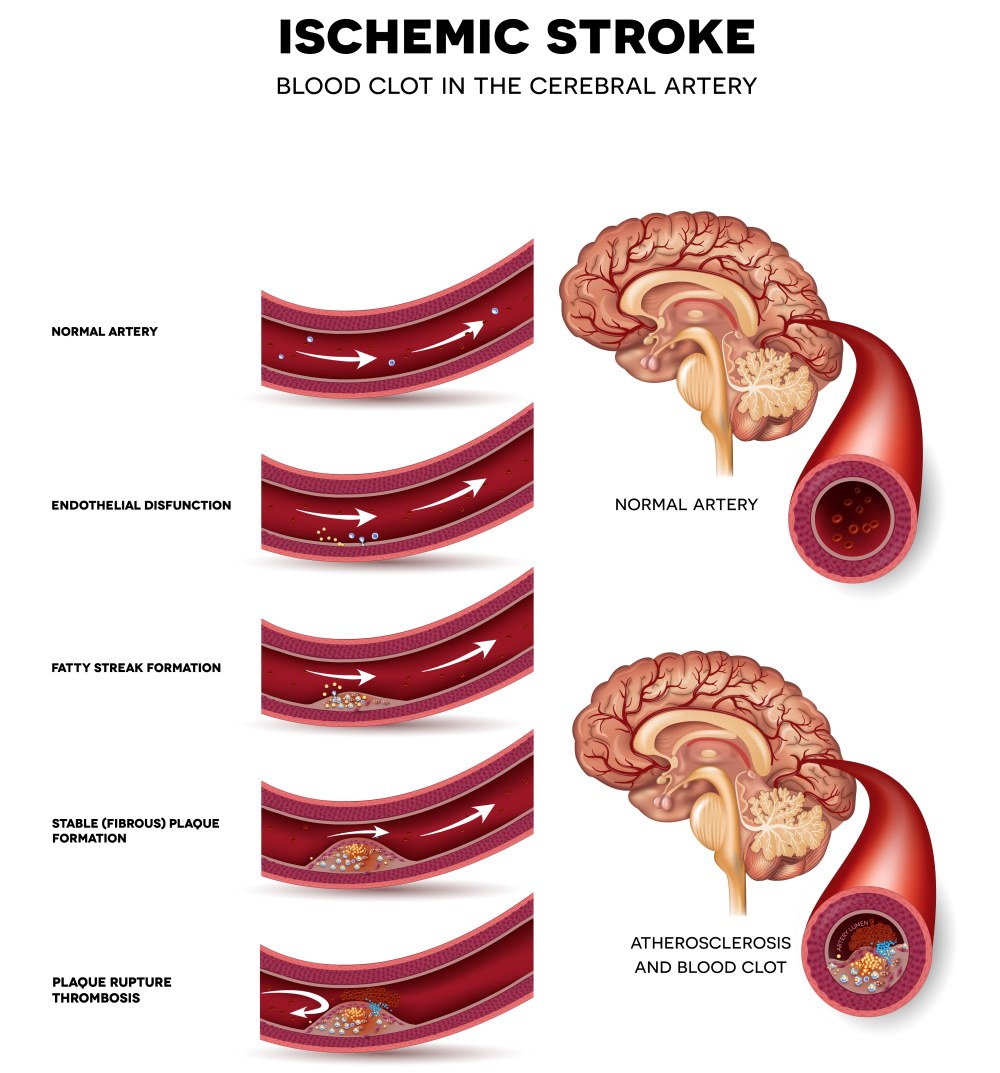
- atherothrombotic: in the lumen of large arteries an atherosclerotic plaque grows, which ulcerates and blood clots form on it. If a plaque ruptures, an arterio-arterial embolism develops;
- hemodynamic: stroke develops against the background of severe stenosis of 70% of both intracranial and extracranial vessels in combination with a sharp fall blood pressure;
- hemorheological: thrombosis in the vessels of the brain occurs as a result of hematological diseases (hypercoagulation of blood - erythremia, thrombocythemia, etc.);
- lacunar infarction: thrombosis of cerebral arterioles in the subcortical nuclei. The lesion is on average 15 mm, but is characterized by its own clinic, therefore it is separated into a separate group.
Depending on which vascular system is affected, the following strokes are distinguished:
- Carotid basin:
- internal carotid artery;
- anterior cerebral artery;
- middle cerebral artery.
- Vertebrobasilar basin:
- vertebral artery;
- basilar artery;
- cerebellar infarction;
- posterior cerebral artery;
- thalamic infarction.
- What is Ischemic Stroke
- Treatment of Ischemic Stroke
- Prevention of Ischemic Stroke
- Which doctors should you contact if you have an ischemic stroke?
What is Ischemic Stroke
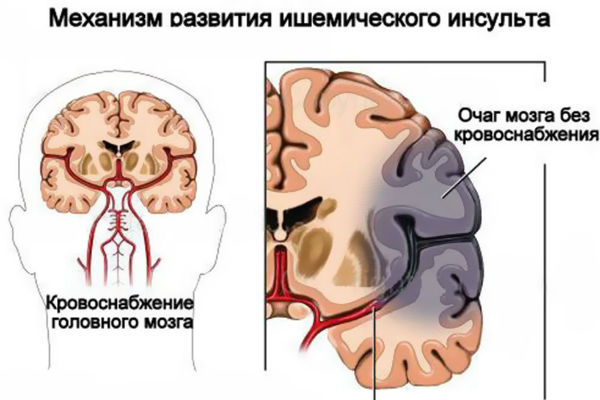
Ischemic stroke is a clinical syndrome manifested by an acute disturbance of local brain functions that lasts more than 24 hours, or leading to death, can be caused either by insufficiency of blood supply in a certain area of the brain as a result of decreased cerebral blood flow, thrombosis or embolism associated with diseases of the blood vessels, heart or blood.
What causes ischemic stroke
Among the main etiological factors leading to the development of ischemic stroke (IS), atherosclerosis, arterial hypertension and their combination should be noted. The role of factors that contribute to increasing the coagulation properties of blood and increasing its aggregation is also extremely important. shaped elements. The risk of IS increases in the presence of diabetes mellitus, myocardial diseases, especially those accompanied by disorders heart rate.
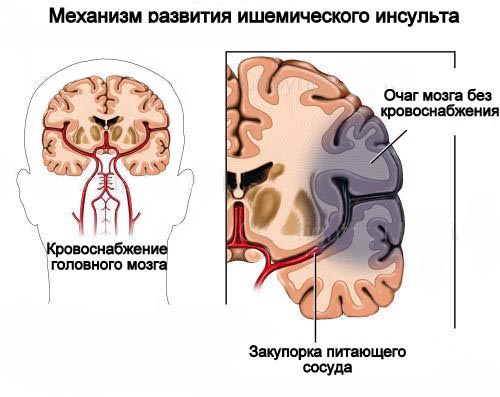
Pathogenesis (what happens?) during ischemic stroke
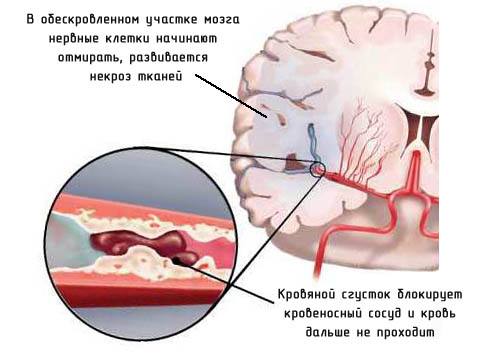
One of the most important pathogenetic mechanisms of development non-thrombotic AI is a narrowing of the lumen of the main arteries of the head or intracranial vessels due to atherosclerosis. The deposition of lipid complexes in the intima of the artery leads to damage to the endothelium, followed by the formation of an atheromatous plaque in this area. In the process of its evolution, the size of the plaque increases due to the sedimentation of formed elements on it, while the lumen of the vessel narrows, often reaching the level of critical stenosis or complete occlusion. Most often, the formation of atherosclerotic plaques is observed in the bifurcation zones of large vessels, in particular the carotid arteries, near the mouth of the vertebral arteries. Narrowing of the lumen of the cerebral arteries is observed with inflammatory diseases- arteritis. In a significant number of cases, congenital structural anomalies are observed vascular system brain in the form of hypoor aplasia of blood vessels, their pathological tortuosity. In the development of IS, extravasal compression of the vertebral arteries against the background of pathologically altered vertebrae is of a certain importance. Damage to small-caliber arteries and arterioles is observed in diabetes mellitus and arterial hypertension.
The existence of a powerful collateral circulation system makes it possible to maintain a sufficient level of cerebral blood flow even in conditions of severe damage to one or two main arteries. In the case of multiple vascular lesions, compensatory capabilities turn out to be insufficient, and the prerequisites for the development of AI are created. The risk of IS increases with impaired autoregulation of cerebral circulation. In this situation important factor, leading to acute cerebral ischemia, is the instability of blood pressure with its fluctuations both in the direction of significant increase and decrease. In conditions of severe stenotic lesions of the cerebral arteries, arterial hypotension, both physiological (during sleep) and developing against the background pathological conditions(acute myocardial infarction, blood loss), is pathogenetically more significant than moderate arterial hypertension
Symptoms of Ischemic Stroke
Clinical picture Ischemic stroke is represented by symptoms of sudden loss of function of a certain part of the brain. They are determined by the part of the brain that is affected by ischemia and the volume of damage. In most cases, the symptoms that patients experience are disturbances in speech, motor and sensory functions, and vision on one side.
- Movement disorders
Weakness or awkwardness of movements on one side of the body, complete or partial (hemiparesis). Simultaneous bilateral development of weakness in the limbs (paraparesis, tetraparesis). Swallowing disorders (dysphagia). Coordination problems (ataxia).
- Speech disorders
Problems understanding or using language (aphasia). Disorders of reading (alexia) and writing (agraphia). Counting disorders (acalculia). Slurred speech (dysarthria).
- Sensory disorders
Somatosensory changes in sensitivity on one side of the body, complete or partial (hemihypesthesia). Visual - decreased vision in one eye, complete or partial (transient monocular blindness). Loss of the right or left half (or quadrant) of the visual field (hemianopsia, quadrant hemianopsia). Bilateral blindness. Double vision (diplopia).
- Vestibular
Feeling of objects rotating (systemic dizziness).
- Behavioral and cognitive disorders
Difficulty getting dressed, combing your hair, brushing your teeth, etc.; violation of orientation in space; problems copying patterns such as a clock, a flower, or intersecting cubes (visuospatial processing disorders). Memory impairment (amnesia).
Diagnosis of Ischemic Stroke
The decision about the need for examination and the choice of methods depend on the patient's symptoms, his age, and the diseases that the patient suffered before and after the stroke; the patient's willingness to accept risk, expense, and inconvenience; the objectives of the survey and the relationship between its cost and effectiveness. However, all stroke patients who undergo intensive therapy, it is necessary to carry out a list of essential examinations, even if the examination clearly indicates the cause of the disease.
Studies that should be carried out for all stroke patients:
- Clinical blood test
- Blood glucose, urea and blood electrolytes
- Blood plasma cholesterol level
- 12-channel electrocardiography
- Emergency non-contrast computed tomography (CT) of the brain for: - for differential diagnosis hemorrhagic stroke and cerebral infarction (CT scan should be performed within a few hours after the stroke)
Patients in whom the etiology of stroke remains unclear or in whom, according to examination or simple methods examinations may suggest a cause, more specialized studies are carried out.
- Ultrasonic duplex scanning
- Cerebral angiography
- Magnetic resonance angiography (MRA) and intra-arterial digital subtraction angiography (IDASA)
- Transthoracic echocardiography (TT-ECHO-CG)
- Magnetic resonance imaging
Treatment of Ischemic Stroke
In the treatment of stroke, it is customary to distinguish between basic and differentiated therapy. Basic therapy does not depend on the nature of the stroke (ischemic or hemorrhagic). Differentiated therapy, on the contrary, is determined by the nature of the stroke.
Basic therapy for ischemic stroke
Basic therapy for stroke is essentially aimed at maintaining basic vital important functions body. Basic therapy includes ensuring adequate breathing, maintaining blood circulation, monitoring and correcting water and electrolyte disturbances, reducing cerebral edema, preventing and treating pneumonia.
Differentiated therapy in the acute period
Epidemiological studies indicate that at least 70% of ischemic strokes are associated with thrombosis or thromboembolism of the cerebral arteries. In these cases, most modern method treatment is the so-called thrombolysis, which is achieved by intravenous or intra-arterial administration of tissue plasminogen activator.
To date, the beneficial effect of thrombolysis on the outcome of ischemic stroke has been proven both in controlled studies and in everyday clinical practice.
In order to improve the rheological properties of blood in the acute period, hemodilution in the form of intravenous infusions. The so-called vasoactive drugs (pentoxifylline, instenon, vinpocetine, blockers) are widely used empirically. calcium channels), although there is currently no evidence of their clinical effectiveness.
Management of patients during the recovery period of ischemic stroke
As a rule, with a favorable course of ischemic stroke, following acute occurrence neurological symptoms, their stabilization and gradual regression occurs. It is assumed that the basis for reducing the severity of neurological symptoms is the process of “retraining” of neurons, as a result of which intact parts of the brain take over the functions of the affected parts.
There is no doubt that active motor, speech and cognitive rehabilitation during the recovery period of ischemic stroke has a beneficial effect on the process of “retraining” of neurons and improves the outcome. Rehabilitation measures should begin as early as possible and be systematically carried out at least during the first 6-12 months after an ischemic stroke. During these periods, the rate of restoration of lost functions is maximum. However, it has been shown that rehabilitation measures have positive effect and at a later date.
For any pathogenetic variant, from the first hours of the manifestation of clinical symptoms, it is necessary to prescribe antiplatelet drugs, which reduces the risk of recurrent ischemic events by 20-25%.
Further prevention of recurrent ischemic strokes should be aimed at correcting the main risk factors for cerebral ischemia. Adequate antihypertensive therapy should be carried out, the patient should be encouraged to stop smoking or reduce the number of cigarettes smoked, metabolic disorders (hypergycemia, hyperlipidemia) should be corrected, and excess weight and physical inactivity should be combated.
Well rehabilitation treatment patients who have had a stroke includes therapeutic exercises, exercises on simulators for passive and active rehabilitation, sling simulators for ergotherapy, massage, hardware verticalization and locomotor exercises (gait restoration), physiotherapy, stimulation treatment, selection of prosthetic and orthopedic devices.
Therapeutic measures in case of acute stroke, it should be started as early as possible, preferably within the “therapeutic window” - in the first 3-6 hours from the moment of development of the disease. Their adequacy to the patient’s condition and intensity largely determine the further course and outcome of the disease. Patients are advised to be hospitalized in a neurological or neurovascular hospital, or in the case of a major stroke - in the intensive care unit. Considering high frequency combinations of vascular damage to the brain and heart, most patients require consultation with a cardiologist. As much as possible early dates the question of the need and possibility of neurosurgical treatment should be resolved. It is inappropriate to hospitalize patients in a state of deep coma with disorders of vital functions, severe organic dementia, incurable oncological diseases.
Patients with PMN require bed rest until completion. acute period and stabilization of the condition. Inpatient treatment is indicated in the case of acute hypertensive encephalopathy, severe hypertensive crisis, and repeated TIAs. Indications for hospitalization are also the lack of effect from outpatient therapy and exacerbation of concomitant diseases, in particular IHD.
There are two main directions of treatment - differentiated, depending on the nature of the stroke (hemorrhagic or ischemic) and undifferentiated (basic), aimed at maintaining vital functions and correcting homeostasis.
Undifferentiated treatment. Correction of the cardiovascular system is primarily aimed at controlling blood pressure. Its numbers should be 15-25 mm Hg. Art. exceed what is usual for the patient. Rare decreases in blood pressure should be avoided to avoid the development of steal syndrome. Antihypertensive therapy includes the use of beta blockers (anaprilin, atenolol), calcium channel blockers (both short-acting - nifedipine and long-acting - amlodipine), diuretics (furosemide), and, if necessary, ACE inhibitors (captopril, enalapril). If oral administration is impossible or ineffective, drugs are administered intravenously under blood pressure control. If arterial hypotension develops, cardiotonic drugs (mesaton, cordiamine) are prescribed; if there is no effect, intravenous corticosteroids (hydrocortisone, dexamethasone) are prescribed. If indicated, correction of coronary circulatory disorders, acute cardiac arrhythmia and conduction disturbances, and heart failure is carried out.
Monitoring respiratory function includes ensuring patency respiratory tract toilet of the oral and nasal cavity, removal of secretions and vomit from the upper respiratory tract using suction. Intubation and transfer of the patient to artificial ventilation lungs. With the development of pulmonary edema, the administration of cardiac glycosides (corglycone, strophanthin) and diuretics is required. In case of severe stroke, antibiotics should be started from the first day wide range actions (synthetic penicillins, cephalosporins) for the prevention of pneumonia. In order to prevent congestion in the lungs, it is necessary to begin active and passive (including turning over from side to side) as early as possible. breathing exercises.
To maintain homeostasis, it is necessary to administer an adequate amount of saline solutions (2000-3000 ml per day in 2-3 doses): Ringer-Locke, isotonic sodium chloride solution, 5% glucose solution, while it is necessary to control diuresis and expiratory fluid losses. Considering that patients with stroke often develop acidosis, the use of 4-5% sodium bicarbonate solution, 3.6% trisamine solution is indicated (under the control of CBS indicators). If necessary, the content of potassium and chlorine ions in the blood is adjusted. In the acute period of stroke, patients should receive a diet rich in vitamins and proteins, low in glucose and animal fats. For swallowing problems, food is administered through a nasogastric tube.
The fight against cerebral edema includes the use of corticosteroids, primarily dexazone (16-24 mg per day, 4 injections) or prednisolone (60-90 mg per day). Contraindications to their use are intractable arterial hypertension, hemorrhagic complications, severe forms diabetes mellitus Glycerol perosa is also indicated for intravenous drip administration of osmotic diuretics (15% solution of mannitol, reogluman) or saluretics (furosemide).
Control for vegetative functions includes regulation of intestinal activity ( rich in fiber and lactic acid products diet, if necessary - the use of laxatives, cleansing enemas) and urination. If necessary, catheterization is performed Bladder, prescribing uroseptics to prevent ascending infection urinary tract. Regular treatment is required from the first day skin antiseptic drugs to prevent bedsores, it is advisable to use functional anti-bedsore mattresses. For hyperthermia, use antipyretics
Differentiated treatment. The main directions of differentiated therapy for acute cerebrovascular accidents are restoration of adequate perfusion in the ischemic penumbra zone and limiting the size of the ischemic focus, normalization of rheological and coagulation properties of blood, protection of neurons from the damaging effects of ischemia and stimulation of reparative processes in nervous tissue.
One of the most effective methods of treatment is hemodilution - the administration of drugs that reduce the level of hematocrit (up to 30-35%). For this purpose, rheopolyglucin (reomacrodex) is used, the daily volume and rate of administration of which is determined by both hematocrit indicators and blood pressure levels and the presence of signs of heart failure. For low blood pressure, it is possible to use polyglucin or isotonic saline solutions. At the same time, solutions of aminophylline, pentoxifylline (Trental), and nicergoline (Sermion) are prescribed intravenously. In the absence of heart rhythm disturbances, vinpocetic (Cavinton) is used. As the patient's condition stabilizes, intravenous administration of drugs is replaced by oral administration. The most effective are acetylsalicylic acid(1-2 mg/kg body weight), it is advisable to use forms of the drug. having a minimal negative effect on the gastric mucosa (thromboass): pentoxifylline, cinnarizine, prodectin (anginin).
In the case of increasing thrombosis of the cerebral arteries, with a progressive course of stroke, cardiogenic embolism, the use of anticoagulants is indicated. Heparin is administered intravenously into daily dose 10-24 thousand units or subcutaneously 2.5 thousand units 4-6 times a day. When using heparin, mandatory monitoring of the coagulogram and bleeding time is necessary. Contraindications to its use, as well as thrombolytics, is the presence of sources of bleeding of various locations ( peptic ulcer stomach, hemorrhoids), persistent intractable hypertension (systolic pressure above 180 mm Hg), severe disorders of consciousness. With the development of DIC syndrome, due to a decrease in the level of antithrombin III, administration of native or fresh frozen blood plasma is indicated. After stopping the administration of heparin, indirect anticoagulants (phenyline, syncumar) are prescribed with monitoring of blood coagulation parameters.
The established nature of the thrombotic stroke allows the use of thrombolytics (urokinase, streptase, streptokinase) in the first hours of the disease. Due to the fact that when intravenous administration These drugs have a high risk of hemorrhagic complications, the most effective way is targeted thrombolysis, in which the drug is injected directly into the area of thrombosis under x-ray control. Recombinant tissue plasminogen activator has a powerful fibrinolytic effect, the administration of which is also advisable only in the first hours of the disease.
IN complex treatment patients with acute disorders cerebral circulation, the use of drugs that have antiplatelet and vasoactive effects is indicated: calcium channel blockers (nimotop, flunarizine), vasobral, tanakan. The use of angioprotectors is justified: prodectin (anginin). The use of these drugs is advisable after the acute phase of the disease has passed, as well as in patients with TIA.
In order to prevent hemorrhage in the ischemic zone during extensive heart attacks Dicinone (sodium etamsylate) is prescribed intravenously or intramuscularly.
The use of drugs that have a neurotrophic and neuroprotective effect on brain tissue is extremely important. For this purpose, use nootropil (up to 10-12 g per day), glycine (1 g per day sublingually), aplegin (5.0 ml in 200.0 ml of isotonic sodium chloride solution intravenously 1-2 times a day), Semax (6-9 mg 2 times a day intranasally), Cerebrolysin (10.0-20.0 ml per day intravenously). The use of these drugs contributes to a more complete and rapid restoration of impaired functions. In some cases, in particular with global cerebral ischemia, it is possible to use barbiturates (sodium thiopental) to reduce the energy needs of the brain under ischemic conditions. The widespread use of this method is limited by the pronounced cardiodepressive and hypotensive effects of the drug and depression of the respiratory center. A certain effect is achieved by drugs that inhibit lipid peroxidation processes: unithiol, vitamin E, aevit.
Prevention of ischemic stroke includes correction of blood pressure, normalization lipid spectrum blood, when blood viscosity increases, antiplatelet agents are prescribed. Diet therapy, dosed, is of great importance exercise stress, rational employment. One of the effective methods for preventing ischemic stroke is surgical reconstruction of the arteries supplying blood to the brain, primarily the carotid, as well as the vertebral, subclavian and innominate arteries. The indication for surgery is severe arterial stenosis, manifested by transient cerebrovascular accidents. In some cases, indications arise for restoring arterial patency in asymptomatic stenoses.
Differentiated conservative treatment with hemorrhagic stroke. The main direction is to reduce the permeability of the vascular wall and prevent the lysis of a formed thrombus. To inhibit fibrinolysis and activate thromboplastin production, epsilon-aminocaproic acid is used. Over 3-5 days, 50.0-100.0 ml of a 5% solution of the drug is administered intravenously 1 or 2 times a day. Inhibitors of proteolytic enzymes are used: trasylol (contrical, gordox) in an initial dose of 400-500 thousand units per day, then 100 thousand units 3-4 times a day intravenously. An effective hemostatic drug with a low risk of thrombosis is dicinone (sodium etamsylate). To prevent vasospasm, which complicates the course of subarachnoid hemorrhage, patients are prescribed Nimotop.
Surgical treatment for hemorrhagic stroke. Removal of medial hematomas, typical for hemorrhagic stroke, localized in the subcortical ganglia, internal capsule, and thalamus, as a rule, does not lead to an improvement in the condition of patients and does not significantly change the prognosis. Only sometimes indications for surgery may arise in patients with relatively young with an increase in cerebral and focal symptoms after a period of relative stabilization. In contrast, removal of hematomas localized in the white matter of the cerebral hemispheres lateral to the internal capsule, as a rule, leads to a significant improvement in the patient’s condition and regression of dislocation symptoms, and therefore surgical intervention for these hematomas it should be considered absolutely indicated.
Main method surgical treatment Craniotomy is used to remove intracerebral hematomas. If the hematoma is located laterally and extends to the insula, the least traumatic approach to the hematoma is through the lateral (Sylvian) fissure, with trepanation performed in the frontotemporal region. Hematomas localized in the area of the visual thalamus can be removed through an incision in the corpus callosum. For atypical hemorrhages surgical approach determined by the location of the hematoma in the brain.
To remove deep-seated hematomas, stereotactic aspiration can be used. Based on the results of a CT study, the coordinates of the hematoma are determined. Using a stereotactic apparatus fixed on the patient's head, a special cannula connected to an aspirator is inserted through the burr hole. In the lumen of the cannula there is a so-called Archimedes screw, the rotation of which leads to the destruction and removal of the hematoma. The advantage of this method is its minimal trauma.
Hemorrhage into the cerebellum can cause life-threatening compression of the brainstem, making surgery necessary. Resection trepanation of the posterior cranial fossa. The dura mater is subsequently opened and the cerebellar tissue is dissected, and the accumulated blood is removed by aspiration and washing the wound.
Ischemic stroke- focal cerebral infarction, manifested by neurological disorders lasting more than 1 hour. The most common reasons ischemic stroke are non-thrombotic occlusion of small, deep cortical arteries; blockage of the cerebral artery by emboli of cardiac or arterial origin; arterial thrombosis with hemodynamic disturbances, leading to a decrease in cerebral blood flow. The diagnosis is made on the basis of clinical data and is confirmed by specifying the extent of the lesion with the results or. In some cases, thrombolytic therapy is effective in the acute period. Measures to reduce the risk of recurrent strokes include carotid endarterectomy, anticoagulant and antithrombotic therapy.
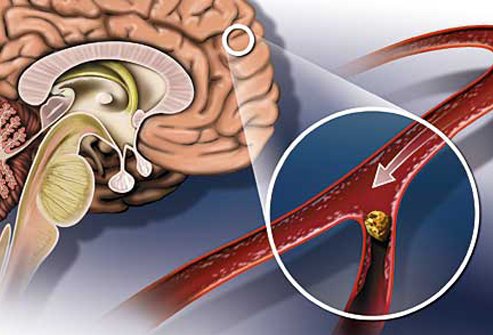
Causes of ischemic cerebral stroke
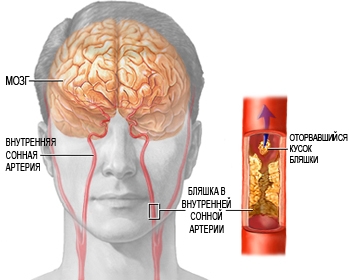
Ischemia usually occurs due to thrombosis or embolism. An ulcerated atherosclerotic plaque is a source for thrombus formation. The formation of an atherosclerotic plaque is possible in any of the large cerebral arteries, but is more common in areas of turbulent blood flow, especially in the bifurcation area carotid artery and in the branches of the internal carotid artery. Most often, blood clots form in the main trunk of the middle cerebral artery and its branches, as well as large arteries of the base of the brain, deep perforating arteries and small cortical branches. The basilar artery and supraclinoid division of the internal carotid artery are often affected, i.e. its segment between the cavernous sinus and the supraclinoid process.
More rare reasons thrombosis may be secondary inflammation of the cerebral arteries due to acute or chronic meningitis, vasculitis of various etiologies; syphilis; dissection of the wall of the cerebral arteries or aorta; diseases accompanied by hypercoagulation or increased blood viscosity; rare diseases, such as moyamoya disease, Binswanger disease; use of sympathomimetic drugs. Early generations of oral contraception were also associated with increased risk thrombosis of cerebral vessels.
An embolus migrating in the bloodstream can temporarily or permanently block any vessel of the arterial tree of the brain. The most common source of cerebral emboli are blood clots that form in the heart during atrial fibrillation, after acute heart attack myocardium or surgery open heart; due to valve damage due to rheumatic heart disease; the source of emboli can be vegetations on the valve leaflets during bacterial or maranthic endocarditis or after valve replacement surgery. The source of emboli is often atheromas of extracranial vessels - the aortic arch and neck vessels. Much less often, embolism is fatty, gas or venous thrombi, which pass from the right half of the heart to the left through an open oval window. Emboli break off spontaneously or after invasive manipulation of the heart and blood vessels.
Small outbreaks ischemic lesion after lacunar infarctions are caused by obstruction of small perforating arteries that supply blood to deep cortical structures. It is believed that the cause of obstruction of these vessels is lipohyalinosis, and not atheromatosis, the role of emboli in occlusion of perforating arteries is highly controversial. Lacunar infarctions occur more often in older people with inadequately controlled diabetes mellitus and arterial hypertension.
Less commonly, ischemic cerebral stroke occurs due to vascular spasm or venous infarction.
Causes of ischemic cerebral stroke
Insufficient blood flow in a single cerebral artery can often be compensated by the effective functioning of the collateral system, especially between the carotid and vertebral arteries through anastomoses in the arterial circle of the cerebrum and, to a lesser extent, between the large arteries of the cerebral hemispheres. However, anatomical variations in the cerebral arterial circle and collateral vessel diameter, atherosclerosis, and other acquired arterial lesions can interrupt collateral flow, increasing the likelihood that occlusion of a single artery will cause cerebral ischemia.
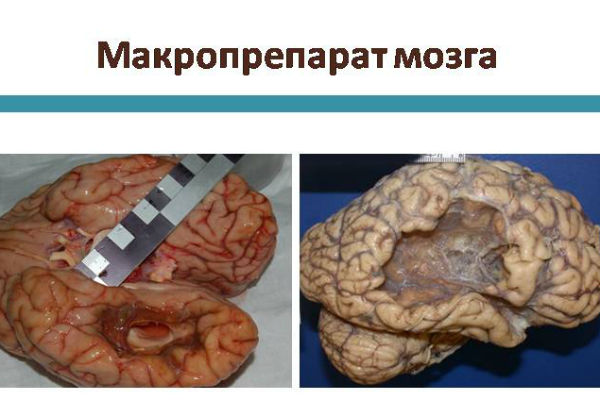
Damage becomes irreversible if blood flow is reduced to less than 5% for 30 minutes or less than 40% for more than 3-6 hours. Damage develops more quickly in hyperthermia and more slowly in hypothermia. If the tissue is in a state of ischemia, but the damage is still reversible, the restoration of blood flow can prevent tissue necrosis or reduce its volume. Otherwise, the mechanisms of ischemic damage are activated - edema, capillary thrombosis, programmed cell death and infarction with cell necrosis. The development of edema and capillary thrombosis is mediated by inflammatory mediators; pronounced or extensive swelling leads to increased intracranial pressure. Necrotic cell death is caused by a decrease in ATP reserves, disruption of ionic homeostasis, peroxidation of cell membrane lipids by free radicals, the action of excitatory neurotoxins and intracellular acidosis due to the accumulation of lactate.
Clinical picture of ischemic stroke
Neurological symptoms depend on the location of the infarction. The clinical picture often makes it possible to determine which artery is affected, but, as a rule, there is no complete match.
In the case of embolism, acute neurological deficits develop within minutes. Thrombotic disorders are characterized by gradual development stroke, sometimes within 24-48 hours, called “stroke in progress”. In the case of a major stroke, unilateral neurological symptoms increase over several hours, gradually taking over all most the corresponding half of the body; the spread of paresis is usually not accompanied by headache, fever or pain in the affected parts of the body. The progression of symptoms is usually stepwise, alternating with periods of stabilization. A stroke is considered subtotal if there is residual function in the affected area.
Cerebral embolism with the development of stroke occurs more often in daytime, the appearance of neurological symptoms is often preceded by. The formation of a blood clot usually occurs at night, so the patient notices neurological symptoms after waking up. With a lacunar infarction, one of the classic focal lesion syndromes develops, while there are no symptoms of cortical damage. The consequence of repeated lacunar infarctions may be the development of post-infarction dementia.
The increase in focal neurological deficit and impairment of consciousness during the first 2-3 days is often caused by increasing cerebral edema, but can also be associated with an expansion of the infarction zone. If the infarction is small, functional improvement is noticeable already in the first days of the disease; further recovery occurs more gradually, over a period of several months to 1 year.
Ischemic cerebral stroke: diagnosis
The diagnosis of stroke should be assumed when there is a sudden onset of neurological disorders corresponding to the blood supply zone of one of the cerebral arteries. Ischemic stroke must first be differentiated from diseases accompanied by similar symptoms, hemorrhagic stroke. Headache, coma or stupor, vomiting are rather symptoms hemorrhage rather than ischemia.
Although a preliminary diagnosis is made by clinical symptoms, CT or MRI and determination of serum glucose levels are the next urgent measures. First, a CT scan is performed to rule out cerebral hemorrhage, subdural or epidural hematoma, and a rapidly growing or suddenly acute tumor. CT signs of even an extensive ischemic stroke in the area of the anterior vascular system may be minimal for several hours: smoothness of the sulci and convolutions of the cortex, absence of a transition zone between the cortex and the white matter, compaction of the middle cerebral artery. After 24 hours of ischemia, infarcts are usually visualized as areas of reduced density, with the exception of small infarcts of the pons and medulla oblongata, which may be hidden by bone artifacts. Diffusion-weighted MRI and magnetic resonance angiography can be performed immediately after CT.
Clinical differences between lacunar, embolic and thrombotic stroke are not reliable, so they are prescribed additional research to identify frequent or removable reasons and risk factors. These include carotid duplex ultrasonography, ECG, transesophageal echocardiography, clinical and biochemical tests blood. In most cases, the research plan is supplemented with magnetic resonance or CT angiography. Narrowly focused studies, such as the determination of antiphospholipid antibodies, are performed depending on the specific clinical situation.
Prognosis for treatment of ischemic cerebral stroke
Stroke severity and prognosis are often assessed using standardized measures, one of which is the Stroke Scale. National Institute health; the indicator on this scale reflects the severity functional disorders and forecast.
In the first days further development The disease and its outcome are difficult to predict. Elderly age, impaired consciousness, aphasia, and signs of brainstem lesions are poor prognostic indicators. Early improvement and younger age make the prognosis more favorable.
Approximately half of the patients with moderate or severe hemiparesis, as well as the majority of patients with a less pronounced neurological defect, experience sufficient functional recovery, they no longer need basic care, and they adequately perceive the world and can move independently, despite incomplete recovery. Complete recovery of the neurological deficit is observed in approximately 10% of patients; most disorders do not recover even after a year, therefore, the function of the affected limb will be limited. Ischemic strokes are prone to recurrence, with each recurrent stroke usually worsening the existing neurological deficit. About 20% of patients die in hospital, and the mortality rate increases with age.
Ischemic cerebral stroke: treatment in the acute period of the disease
Patients in the acute period of ischemic stroke are treated with inpatient conditions. During initial examination To stabilize the patient's condition, as a rule, symptomatic therapy. To ensure adequate perfusion of the ischemic area of the brain in conditions of impaired brain autoregulation mechanisms, increased blood pressure is required. In this regard, blood pressure is not reduced if systolic does not exceed 220 mm Hg. Art., and diastolic - 120 mm Hg. Art. according to two consecutive measurements with an interval of more than 15 minutes, provided that the patient has no signs of damage to other target organs and treatment with recombinant tissue plasminogen activator is not planned. To relieve arterial hypertension, nicardipine is administered intravenously at a dose of 5 mg/hour, then the dose is increased by 2.5 mg/hour every 5 minutes until maximum dose 15 mg/h required to reduce systolic blood pressure by 10-15%. Alternatively, labetalol is given intravenously.
Antithrombotic therapy may include tissue plasminogen activator, thrombolysis, antiplatelet agents, and anticoagulants. For most patients, thrombolytic therapy is not indicated due to various reasons, therefore, we have to limit ourselves to antiplatelet therapy, which is critical in the first 24-48 hours. Contraindications to the prescription of aspirin and other antiplatelet agents are allergies to NSAIDs, especially asthma and urticaria, any types allergic reactions to aspirin or tartrazine, acute gastrointestinal bleeding, G6PD deficiency and warfarin use.
Recombinant tissue plasminogen activator is used in the first 3 hours of the acute period of ischemic stroke if the patient does not have any contraindications. It should not be forgotten that tissue plasminogen activator can cause cerebral hemorrhage with associated consequences, which can sometimes be fatal. At the same time, treatment with tissue plasminogen activator in strict accordance with the protocol significantly increases the likelihood of functional recovery of the patient. Treatment with tissue plasminogen activator should only be performed by physicians experienced in the treatment of acute strokes; lack of experience is fraught with violation of the treatment protocol with its consequences in the form of cerebral hemorrhage and death of the patient. One of the most difficult requirements of the tPA treatment protocol is the administration of the drug no later than the first 3 hours from the onset of the disease. Exact time the appearance of symptoms can rarely be established; In addition, before starting treatment, it is necessary to conduct a CT examination to exclude hemorrhage, and then exclude all possible contraindications to the use of tissue plasminogen activator. The recommended dose of tPA is 0.9 mg/kg; 10% of the dose is administered intravenously quickly, the remaining part is administered by long-term infusion. After the administration of tPA, continuous monitoring of vital functions is carried out in the next 24 hours. After using tPA, the use of any anticoagulants and antithrombotic drugs is excluded for the next 24 hours. In case of bleeding, immediate intensive treatment is started.
Thrombolysis of a thrombus or embolus n stu is indicated for extensive stroke and the appearance of the first symptoms in the interval from 3 to 6 hours before the intervention, primarily in case of occlusion of the middle cerebral artery. This treatment is standard in some large clinics, but not available in most others.
Treatment of ischemic cerebral stroke heparin or low molecular weight heparins is indicated in cases of cerebral venous thrombosis or embolic stroke due to atrial fibrillation, in cases of progression of thrombosis during treatment with antiplatelet agents and when it is impossible to use other treatment methods. At the same time with parenteral administration heparin is prescribed warfarin orally. Before starting anticoagulant treatment, a CT scan is performed to exclude hemorrhage. Continuous infusion of heparin is carried out in cases where the partial thromboplastin time needs to be increased by 1.5-2 times from the initial values, until during treatment with warfarin the MHO increases to 2-3.
Warfarin increases the likelihood of bleeding, so it should only be prescribed to patients who are able to comply with the dosage regimen and control measures, and who are not prone to falls and potential injuries.
Long-term therapy of ischemic stroke.
Symptomatic therapy continues throughout the entire period of convalescence and rehabilitation. Control of common medical risk factors helps limit the area of brain damage after stroke, leading to better functional recovery.
Carotid endarterectomy surgery is indicated for patients with carotid artery stenosis who have recently suffered minor strokes or TIAs without residual neurological defect. In patients with neurological symptoms, endarterectomy, with or without antiplatelet therapy, is indicated for obstruction of more than 60% of the lumen, with or without ulcerated plaque, and with a life expectancy of at least 5 years. The manipulation can only be performed by highly qualified surgeons with an individual rate of complications and mortality when performing such an operation of less than 3%.
Oral antiplatelet drugs are prescribed to secondary prevention recurrent strokes. Aspirin 81-325 mg once daily, clopidogrel 75 mg once daily or combination drug, containing 25 mg aspirin / 200 mg extended-release dipyridamole. It is advisable to avoid concomitant treatment with warfarin and antiplatelet drugs due to the cumulative increase in the risk of bleeding, however, in high-risk groups, combined treatment with aspirin and warfarin is allowed.
Ischemic stroke is a consequence of such pathologies of the cardiovascular system as thrombosis, embolism in cerebral atherosclerosis, cardiogenic embolism and others. Ischemic stroke, or cerebral infarction, is not considered an independent disease; it is a clinical syndrome manifested sharp decline blood supply to the brain focus and forming an area of necrosis (necrosis) of brain tissue.
Ischemic stroke is accompanied by persistent neurological symptoms: blindness, loss of sensitivity, speech impairment, paresis of body parts, dizziness, which occur instantly and often lead to death.
Ischemic stroke, in contrast to hemorrhagic stroke and subarachnoid hemorrhage, is the most common type of circulatory dysfunction in the brain, recorded in 80% of cases of heart pathology. Its appearance is due to blockage of the lumen of the artery supplying the brain. Lack of blood flow and lack of oxygen to brain tissue kills cells.
In medicine, it is customary to classify ischemic stroke depending on the cause and mechanism of the disease, clinical manifestations, localization of the infarction zone.
Considering the cause and mechanism of occurrence of the pathology, cerebral infarction is classified by type:
- thromboembolic - complete blocking of blood vessels by a thrombus;
- hemodynamic - arterial hypertension and hypotension provoke spasm of cerebral vessels, leading to deficiency nutrients;
- lacunar - constant high pressure causes damage to the arteries, resulting in numbness of the limbs and decreased motor activity.
Depending on the location of the lesion, the following types of ischemia are distinguished:
- transient ischemic attack - disorders localized in a specific focus (for example, blindness in one eye), disappearing after a day;
- minor stroke - a variation of ischemia that restores body functions from 2 to 21 days; progressive gradual appearance of symptoms from several hours to 2-3 days, incomplete restoration of functions;
- Complete or extensive ischemic stroke - a fully formed stroke with long-lasting symptoms.
Ischemic cerebral stroke is diagnosed based on the severity of the disease. mild degree, moderate and severe form.
Ischemic cerebral stroke: causes and diagnosis
 Ischemic cerebral stroke develops as a result of chronic disease arteries (atherosclerosis) and intravascular formation of blood clots (thrombosis), as well as other damage of similar etiology. The causes of the pathology are directly related to the type of ischemic stroke.
Ischemic cerebral stroke develops as a result of chronic disease arteries (atherosclerosis) and intravascular formation of blood clots (thrombosis), as well as other damage of similar etiology. The causes of the pathology are directly related to the type of ischemic stroke.
Thromboembolic stroke occurs due to higher level cholesterol and occurs as a result of embolism - blocking of the vascular lumen by some substance.
Causes of embolism include:
- The development of a plaque in the carotid artery, consisting of cholesterol and blocking the flow of blood to the brain.
- Violation of the structure of the endothelial (vascular) wall, leading to a slowdown in blood circulation and blood thickening - thrombosis. A thrombus also forms in the heart and blood vessels of the legs (thrombophlebitis).
- Damage to tissues along with blood vessels as a result of injuries.
- Vascular spasms that occur due to overwork, hypoxia, vegetative-vascular dystonia, osteochondrosis, bad habits ( nicotine addiction), drug use, lead to vasoconstriction. Often occurs in older people.
- Gas entering vessels.
- Clogged arteries with fat.
- Fractures, neoplasms, operations cervical spine and chest.
- Inflammatory processes, infection.
Hemodynamic ischemic stroke provokes a sharp drop in blood pressure, leading to insufficient blood circulation.
Factors that provoke this condition are:
- impaired blood flow due to acute heart failure, myocardial infarction;
- a drop in vascular tone and blood circulation volume (collapse), which is caused by kinking (kinking) of a vessel, a tumor pressing on the vessel, the formation of a mixture of fats and vessels (plaques);
- a combination of several of the above reasons.
Ischemic lacunar cerebral infarction is associated with increased blood pressure(hypertension) and the resulting pathology of cerebral vessels.
The causes of lacunar stroke are the following diseases:
- high blood sugar;
- hypertension;
- inflammation of the blood vessels in the brain (vasculitis);
- infection of brain tissue (meningitis and the like);
- situations of stress;
- bad habits.
Remember, ischemic stroke of the brain manifests itself when, after improper or untimely treatment of the above diseases, arterial thrombosis, arterial embolism, and atherosclerotic damage to the arteries develop.
To diagnose a cerebral stroke of an ischemic nature, it is necessary to determine the period from which the disruption of blood flow began, establishing the frequency of recurrence and the sequence of manifestation of symptoms. First, you need to pay attention to the expression of neurological symptoms and rule out possible factors risk (hypo-/hyperglycemia, hypertension, arrhythmia and others).
The necessary physical diagnosis (examination to clarify the diagnosis) consists of the following procedures:
- Availability common symptoms- headache, confusion, convulsions and others.
- Presence of neurological and meningeal signs.
- Laboratory research(clinical and biochemical blood tests, general analysis urine, hemostasiogram (test for blood clotting).
- Instrumental diagnosis of cerebral infarction - MRI and CT of the brain.
- Neuroimaging methods make it possible to exclude other manifestations of intracranial pathology and detect the first signs of ischemic brain damage to the head: the absence of an image of the lenticular nucleus or insular cortex, as well as hyperdensity of the cerebral artery on the affected side.
- Computed tomographic signs of ischemic stroke in the area for a short time can be minimally expressed. A day later, heart attacks appear as areas of reduced density.
The main thing is to correctly identify the type of brain pathology. Since their symptoms are similar, it is necessary to distinguish between ischemic and hemorrhagic strokes. You can do this using instrumental diagnostics. These include ultrasonography, ECG, echocardiography, clinical and biochemical blood tests. In most cases, the research plan is supplemented with magnetic resonance or CT angiography. Narrowly focused studies are carried out according to indications.
Ischemic stroke: symptoms and principles of treatment
 Ischemic stroke, the symptoms of which appear before its onset, tends to occur completely unexpectedly. His approaching soon can be identified by certain symptoms. Most often, at first a person may faint (at times this fainting is accompanied by convulsions and disruption of normal breathing), and at times it can even lead to a deterioration in orientation in space, but this is mainly a consequence of fainting.
Ischemic stroke, the symptoms of which appear before its onset, tends to occur completely unexpectedly. His approaching soon can be identified by certain symptoms. Most often, at first a person may faint (at times this fainting is accompanied by convulsions and disruption of normal breathing), and at times it can even lead to a deterioration in orientation in space, but this is mainly a consequence of fainting.
There are also symptoms of ischemic stroke such as headache, nausea, and occasionally vomiting. Depending on the affected artery of a particular vascular system, the patient after fainting appears certain focal neurological signs.
There are several large vascular networks present in the brain:
- The first is the vascular network of the carotid artery, which includes the anterior, middle and posterior arteries. Due to the fact that the blood supply zones of these arteries cross each other, the likelihood of progression of acute vascular failure is reduced.
- The second is the vertebrobasilar vascular network. Supplies blood to areas of the brain, including centers necessary for the continuation of life.
This vascular network supplies blood to the cerebellum, medulla and initial department spinal cord. Based on the existing symptoms, the neurologist is able to accurately identify the large artery with the affected branch.
For example, signs of stroke of the ischemic type of infarction concentrated in the vascular network of the carotid artery are as follows:
- Pathology of movements of the arms and legs.
- A speech disorder in which a person is simply unable to speak.
Similar symptoms occur when a heart attack develops in the dominant (usually left) hemisphere.
If the infarction progresses in the vertebrobasilar vascular network, the patient will experience the following disorders:
- coordination disorder;
- deterioration in pronunciation of certain words and vision;
- difficulty swallowing food.
When the stroke is concentrated in the trunk, the patient develops the following severe symptoms:
- rapid development of paralysis of each limb;
- significant reduction in blood pressure;
- difficult awakening after sleep;
- development of pathology of rhythm and depth of breathing;
- enuresis of urine and feces.
If an ischemic stroke is concentrated in the cerebellum, the symptoms will be as follows:
- headache;
- dizziness;
- inability to simply stand or walk;
- body movements become uncoordinated;
- the eyes begin to move independently and rapidly horizontally or vertically.
Cure from stroke of ischemic type should not be delayed. The treatment itself must be long and timely - this is the only way to partially or completely restore brain activity, as well as prevent unpleasant exacerbations.
First, patients are assigned to special wards of the neurological or intensive care department. Next, doctors are faced with the task of eliminating acute pathologies respiratory and cardiovascular systems. If necessary, intubate is performed and the patient is switched to artificial respiration. Homeostasis, the functioning of blood vessels, the heart and respiration are constantly monitored.
Particular priority is given to reducing intracranial pressure and preventing cerebral edema. Pneumonia, pyelonephritis, thromboembolism and bedsores are prevented.
The most effective method of healing from an ischemic heart attack is thrombolysis, which should be carried out within five hours after the heart attack. This technique assumes that only a portion of the cells are irreversibly damaged. In general, this part of the cells is called the ischemic nucleus. It is surrounded by a zone of disabled cells, which, however, continue their vital functions.
When a person begins to take substances whose effect is to liquefy and dissolve the blood clot, blood flow standardizes and these cells resume their function. Especially used for this purpose medicinal drug- Actilise.
Basically, to cure ischemic stroke, the following are used: anticoagulants, blood thinners, vasoactive substances, antiplatelet agents, angioprotectors, neurotransmitters and antioxidants.
Differences in treatment of left and right side No, but proper treatment requires an individualized approach. In addition, the doctor is required to select a unique combination of medications.
Ischemic stroke: consequences, complications and life after
Ischemic stroke, the consequences of which may appear periodically, serious pathology, after which you need to be very careful about your lifestyle. Any complications of ischemic stroke can regress. In the worst case, a person will receive the first or third group of disability.
 Following the disease there are the following complications:
Following the disease there are the following complications:
- congestive pneumonia;
- cerebral edema;
- heart failure;
- penetration of thromboembolus into the pulmonary artery system;
- bedsores;
- blood poisoning.
For complete healing after an ischemic stroke, proper nutrition is also important. It is recommended to eat approximately four to six times a day. Food should not contain many calories and should be distinguished by the presence large quantity proteins, vegetable fats and complex carbohydrates.
Also very important raw vegetables, because thanks to them, biochemical processes improve. Since cranberries and blueberries help eliminate free radicals quickly, they should also be included in your daily diet.
Key tips: eat less salt, and smoked, fried, fatty and flour foods should be completely removed from the diet.
To minimize the complications of ischemic stroke, long-term rehabilitation is necessary. That is, a complex of various activities, the purpose of which is to ensure social adaptation person. It is significant enough for full recovery after a stroke.
For proper rehabilitation it should be carried out in a special neurological sanatorium.
Rehabilitation includes several procedures:
- physiotherapy;
- massage;
- mud treatment;
- acupuncture.
Thanks to these procedures, the motor and vestibular systems are restored. The help of a neurologist and speech therapist will ensure the restoration of normal speech. It is also advisable to use various medications, which help in brain restoration.
Don't exclude foods like dates and berries. You can drink a tablespoon of onion juice with honey every day after eating. At dawn, drink pine cone liqueur.
Life after an ischemic stroke requires constant monitoring and proper nutrition, good sleep and rest. Prevention includes various methods, the purpose of which is to eliminate the likelihood of a heart attack and various complications after it.
It is very important to promptly treat arterial hypertension, get examined for heart pain, and also exclude sudden increases in blood pressure. Depending on the various factors, life after an ischemic stroke can last several weeks, or maybe more than 10 years.
Ischemic infarction: symptoms and treatment
An ischemic heart attack occurs when there is insufficient blood circulation, since the tissues that form the brain are very sensitive to a lack of oxygen, since they need constant oxygen supply.
Gray matter cells (the basis of the cerebral cortex) are especially sensitive to hypoxia. These cells die within minutes due to lack of oxygen.
 The main symptoms of ischemic infarction include:
The main symptoms of ischemic infarction include:
- feeling of body numbness;
- feeling of weakness and dizziness;
- loss of sensation in the arms and legs;
- severe attack headache;
- difficulties in speech;
- the appearance of impaired coordination;
- feeling a little dazed;
- feeling drowsy;
- the appearance of nausea or vomiting.
With an ischemic heart attack, the person turns pale and there is a decrease in blood pressure. Increased blood pressure occurs infrequently, mainly only with brainstem infarction. The pulse rate increases (but is less full), there is no change in temperature.
If a person has previously had an ischemic heart attack, then a repeated attack (right hemisphere of the brain) can affect mental health. First, clouding of consciousness appears, gradually turning into dementia.
Sometimes, when consciousness is restored, the patient sees hallucinations, is delusional, that is, signs of psychosis appear. Very rarely (in the case of a blood clot in the carotid artery) a person can fall into a coma. Knowing the symptoms of a heart attack makes it possible to identify a heart attack and take urgent measures.
With timely assistance, a cerebrovascular accident of the ischemic type, a heart attack may not lead to disability. During the first 1.5 hours after the impact, the most Negative consequences. Therefore, the greatest effect of treatment appears in the first 2 hours.
A cerebral infarction is emergency patient and should be urgently hospitalized.
In a hospital, the main objectives of treatment are:
- restoration of blood circulation in brain tissue;
- protection against damage to nerve fibers.
Therefore, almost from the first hours of this condition, the doctor prescribes drugs that break up blood clots - thrombolytics. Such drugs are also applicable in the treatment of myocardial infarction. Thrombolytics when dissolving a blood clot prevent damage nerve cells and help reduce the size of the lesion.
Anticoagulants help reduce and stop the growth of existing blood clots and prevent new ones from appearing. In addition, such drugs help reduce blood clotting.
Antiplatelet agents are drugs whose action is aimed at changing the properties of blood. Such drugs stop the adhesive processes (or platelet aggregation). Antiplatelet agents are among the standard agents used for therapeutic methods stroke caused by cerebral atherosclerosis or various diseases blood with the appearance of blood clots. These drugs are also used to prevent the development of a recurrent stroke.
It should be remembered that brain cells will begin to die without nutrition and oxygen enrichment. Biochemical processes begin immediately, which can be stopped with the help of drugs - cytoprotectors or neuroprotectors. The latter help increase the activity of cells surrounded by “dead” cells. “Non-participating” cells at this time take on the mission of dead cells.
During a heart attack there is surgical methods treatments, such as carotid endarterectomy. During the operation, the inner wall of the carotid artery with atherosclerotic plaque is removed. Surgery is the treatment of choice if the cause of the stroke is a blockage in the carotid artery. This method used to prevent a recurrent attack or prevent a stroke.
Patients have hope and chances for effective treatment and recovery after heart attack and stroke. The most important thing is to have patience, courage and strength to achieve a positive result.
Cerebral infarction is a rather scary diagnosis, but this disease often strikes older people whose age has surpassed the 60-year mark. The second name for this disease is ischemic stroke.
Surprising fact: patients who have not complained of arterial hypertension in the past can be susceptible to the disease. If you go to the clinic in a timely manner, the prognosis can be quite favorable - there are cases of 100% recovery of patients.
By studying ischemic stroke in detail, the symptoms and causes of its occurrence, as well as first aid methods, you can one day save not only your own life, but also someone else’s life.
Classification and periodization
The classification of the disease is very extensive. We will briefly go over the types of ischemia to get an overall picture of the lesion. According to duration, the disease is divided into the following types:
- transient ischemic attack (this neurological disorder is focal);
- “minor stroke” (attacks have a prolonged effect and reverse neurological defect);
- progressive ischemic stroke (develops gradually and can last up to several days);
- total ischemia (cerebral infarction is accompanied by a stable-regressive or incomplete deficit).
And here is what the classification of the disease looks like in relation to its severity:
- mild degree - neurological symptoms are minor, regression lasts approximately three weeks;
- average degree- focal symptoms dominate, but obvious disorders of consciousness are not visible;
- severe degree - general cerebral disorders are pronounced, focal deficit has a severe neurological form.
Focusing on the pathogenesis, doctors identified several more manifestations of cerebral infarction.
According to this classification, stroke is divided into:
- atherothrombotic;
- cardioembolic;
- hemodynamic;
- lacunar;
- rheological.
An ischemic cerebral stroke can be located anywhere. Considering the arterial basin, we will highlight several key areas of damage:
- cerebral anterior (middle, posterior) arteries;
- main artery with branches and vertebral arteries;
- internal (carotid) artery.
Ischemia is a complex multi-stage process. The disease can last for years and is divided into five periods:
- acute - manifests itself within three days (the first);
- acute - 28 days (then the next stage begins);
- early - lasts six months, is considered the beginning of recovery;
- late - extends up to 2 years, is part recovery period;
- residual effects are observed after two years.
Causes
Often, cerebral infarction occurs due to blockage of blood flow by an embolus or thrombus. Cerebral circulation is disrupted, and the patient feels the influence of the atherosclerotic process. More often, people who have suffered transient attacks and are now susceptible to arterial hypertension suffer from ischemia.
There is a whole layer of chronic ailments that can lead to ischemia. It is not for nothing that angina pectoris, the treatment of which folk remedies has become widespread, it is considered a wake-up call. Most problems lie in the cardiovascular system.
Here they are:
- increased blood viscosity;
- congenital cardiovascular defects;
- slow blood flow;
- defibrillation (this procedure provokes the separation of blood clots);
- endocarditis (active rheumatic) - affects the left heart valves;
- embedded pacemakers;
- dissecting aortic aneurysm;
- heart failure;
- myocardial infarction;
- lipid metabolism disorder;
- obesity and diabetes;
- atrial fibrillation;
- age (lower threshold - 60 years);
- minor "ischemic stroke";
- physical inactivity;
- bad habits (tobacco, alcohol);
- migraine;
- oral contraceptives;
- hematological diseases (paraproteinemia,).
How to recognize ischemia
The patient may feel the approach of the disease, since ischemic stroke and its symptoms make themselves felt by characteristic ailments:
- dizziness (the eyes become completely dark);
- short-term speech disorders;
- periodic (weakness in an arm or leg, numbness of the entire side of the body);
- vomiting and nausea;
- blurred vision;
- sudden loss self-control;
- curvature of the tongue;
- inability to smile.
Sometimes the patient's face may be slanted - this a clear sign that immediate medical intervention is required.
Symptoms
Speech disorders caused by ischemic stroke are called “aphasia.” There are certain differences in symptoms between left-handers and right-handers - it depends on which hemisphere of the brain is damaged.
Let's list general signs ailments:
- right-sided smoothness of the nasolabial triangle;
- facial distortion (direction depends on the side of the lesion);
- "parusit" right cheek;
- paralysis of limbs;
- left-sided deviation of the tongue.
When the vertebrobasilar vascular system is affected, ischemic stroke and its symptoms become even more diverse:
- coordination and static disorders;
- dizziness (when the head is thrown back and walking, the symptom intensifies);
- oculomotor and visual pathologies;
- dysarthria (a type of aphasia when the patient cannot pronounce individual letters);
- quiet speech;
- hoarse voice;
- dysphagia (difficulty swallowing food);
- paralysis, paresis, distortion of sensitivity (usually affecting the area opposite to the focus of ischemia).
When an artery is blocked, blood stops flowing to the respiratory and vasomotor centers, which leads to a number of bad symptoms:
- loss of consciousness;
- tetraplegia (paralysis of the limbs);
- periodic breathing;
- dysfunction pelvic organs;
- cyanosis of the face and a drop in cardiac activity.
The cerebellum is responsible for coordinating our movements. Therefore, his defeat is fraught with the following consequences:
- instability (the patient falls in the direction of the ischemic focus);
- vomiting and nausea;
- dizziness and acute migraine;
- nystagmus (involuntary and sudden twitching eyeballs);
- inconsistency of movements.
Complications
Ischemic stroke, which has not been properly treated, is fraught with serious complications. Therefore, it is important to recognize the disease early stages and stop its further development.
Here are the most common complications:
- (affects the lower leg area);
- infectious complications (suffers urinary system, bedsores and pneumonia develop);
- swelling of the brain;
- pulmonary thromboembolism;
- disorders of urination and defecation;
- the cognitive dissonance;
- epilepsy (20% of cases);
- mental disorders (irritability, mood swings, depression);
- motor dysfunction (bilateral and unilateral), paralysis, weakness;
- pain syndrome.
Diagnostics
Early diagnosis is a decisive factor in identifying ischemic cerebral stroke and differentiating it from similar diseases (hemorrhagic stroke).
The key diagnostic methods in the early stages are:
- Physical examination. The patient's condition is assessed according to a number of criteria, including breathing and hemodynamic disturbances, differences in pulse and blood pressure.
- Transcranial Dopplerography. This examination indirectly reveals the speed of blood flow in the intracranial arteries.
- Angiography. Considered the most effective method diagnostics, since it detects aneurysms, narrowing of the lumen and other pathologies.
- Echocardiography and ECG. Considered mandatory diagnostic procedure, excludes cardiac pathologies.
- X-ray examination. Not always used, since its main purpose is to identify pulmonary complications(PE, aspiration pneumonia).
- Blood tests . Doctors are interested in biochemical, clinical and gas tests, as well as coagulograms.
Computed tomography and MRI
Acute ischemic stroke is visualized using magnetic resonance imaging. Compared to computed tomography is a more informative diagnostic method. Tomograms record ischemic changes already on the first day of occlusion formation. If the lesion develops in less than 12 hours, half of the tomograms do not reveal catastrophic changes.
Non-contrast CT images may not differentiate between microscopic cerebral infarcts (lacunar and brainstem infarcts).
Differential diagnosis
In some cases, the patient may need lumbar puncture. Before using it, the doctor must make sure complete absence contraindications. Ischemic stroke involves clear cerebrospinal fluid. The content of cellular elements and protein in it will be normal. It is necessary to differentiate a cerebral infarction from two similar strokes:
- subarachnoid hemorrhage;
- cerebral
Treatment
Therapy will depend on the volume, location of the lesion and the patient’s condition. Ischemic stroke and its treatment can be divided into specific and basic therapy. Basic treatment based on a set of measures to ensure the prevention of somatic ailments. The objectives of this therapy are:
- Adjust blood pressure, support the functioning of blood vessels and the heart.
- Normalize respiratory function.
- Stabilize the patient's temperature.
- Regulate homeostasis (acid-base balance, water-salt balance, glucose level).
- Symptomatic treatment.
- Prevention of urinary infections, pulmonary embolism, bedsores, pneumonia, peptic ulcers and limb fractures.
Specific therapy involves the use of fibrinolytic agents, anticoagulants and antiplatelet agents.
First aid
If you encounter someone who has had a stroke, don't panic. You can help him without difficulty, the main thing is to follow the step-by-step instructions.
The steps are:
- Place the patient on his back and provide access to oxygen. To do this you will have to unfasten the collar. Find a pillow (a small bolster will do) to place under the victim's head.
- When salivating (option - mucus), the patient's head must be turned to the side and a napkin placed underneath.
- Reassure the patient. This is done with 1 gram of glycine (the drug is placed in the mouth).
- The patient should not be given medications that lower blood pressure, and injections are also not recommended. If you decide to lower the pressure, then do not go too far (maximum 10-15 units). Row medicines generally contraindicated (nikoshpan, papaverine, a nicotinic acid, but-shpa).
- Call an ambulance or do it yourself intramuscular injection piracetam (10 ml will prevent brain death). Cerebrolysin will also be useful.
Folk remedies
If your relative is struck by angina, treatment with folk remedies will not seem like nonsense, but will become one of the options for saving a person. This harsh truth also applies to cerebral infarction. ethnoscience pursues the following goals:
- decrease in blood pressure;
- restoration of paralyzed limbs;
- from cholesterol plaques.
To restore normal functioning limbs, you can start making ointments based on vegetable oil and Bay leaf. A good option would be bay leaf mixed with juniper and butter. Peony tincture is recommended for internal use.
Also good help There will be honey tinctures created from onion juice, honey and citrus fruits. Famous garlic tincture will also come in handy. All these means are acceptable during the rehabilitation period, when the danger has disappeared and the patient’s body is recovering from the illness.
Prevention
Primary prevention involves addressing the diseases underlying ischemia. Doctors fight against arterial hypertension antihypertensive drugs. The patient also needs blood pressure stabilization for 24 hours. Patients classified as at risk are under constant supervision.
This applies to:
- diabetes mellitus;
- arterial hypertension;
- primary strokes.
Secondary prevention is based on three factors:
- the use of antiplatelet agents (in some cases - anticoagulants);
- stabilization of blood pressure;
- diet (cholesterol should be completely excluded from the diet).
Be prepared to use the following medications:
- cardiomagnyl;
- aspecard;
- Agrenox;
- lipid-lowering drugs (statins and atorvastatins);
- trombonet;
- simvastatins (Simvatin, Liprimar, Vabadin, Torvacard, Atorvacor).
There are also more complex preventive procedures (even classes with a speech therapist). It is better to postpone a cerebral infarction in time than to expose yourself to danger. Try to minimize your cholesterol intake, move more and control your own weight.
And it affected us. Vitya has a stroke.

